The new study, with collaboration from USF Health, establishes potential targets for treating diabetic damage to nerves regulating heart rate
Cardiac autonomic neuropathy, a common complication of diabetes, can increase the risk of severe heart disease, and sudden cardiac death caused by abnormal heart rhythms known as arrhythmias. Earlier research at the USF Health Morsani College of Medicine, University of South Florida, and elsewhere has helped define how diabetes affects innervation of the heart and damages nerves that control involuntary (autonomic) regulation of body functions, including heart rate.
Now a new preclinical study, including USF Health collaborator Sami Noujaim, PhD, has discovered that inhibiting the enzyme glycogen synthase kinase-3B (GSK3ß) in heart muscle cells reduces dysfunctional parasympathetic nervous system activity associated with diabetes. Recently published in PLOS ONE, the Tufts University-led study used a mouse model for type 1 diabetes (Akita mouse) in which the cardiac-specific GSK3ß gene was selectively and partially inactivated.
In particular, the findings support a new mechanism for understanding how overstimulation of GSK3ß in type 1 diabetes affects development of an abnormal cardiac parasympathetic response in diabetes and also suggests new targets for treating or preventing damage to nerves that regulate heart rate.
The sympathetic nervous system, which mobilizes the body’s “fight-or-flight” responses to stress, accelerates heart rate. The “rest-and-digest” parasympathetic nervous system, which helps calm the body, slows heart rate.
These two components of the involuntary nervous system are normally in constant flux. In fact, slight variations in the time between each heartbeat, known as heart rate variability, characterizes a healthy heart in which both sympathetic and parasympathetic systems communicate effectively to maintain regulatory balance. Conversely, in cardiovascular disease and diabetes, heart rate variability decreases.
“Reduced heart rate variability is a harbinger of bad cardiovascular outcomes in the future,” said co-investigator Dr. Noujaim, associate professor of molecular pharmacology and physiology at USF Health. “So, we want to find a signaling pathway to target that can increase heart rate variability. Our goal is to reduce the likelihood of the diabetic heart developing poor cardiovascular outcomes, including arrhythmias.”
Dr. Noujaim directs a cardiac electrophysiology research laboratory, which has the tools to translate mouse heart activity into frequencies used to analyze beat-to-beat variations in heart rate. High frequencies are predominately generated from parasympathetic regulation of heart rate, while low frequencies result largely from sympathetic regulation.
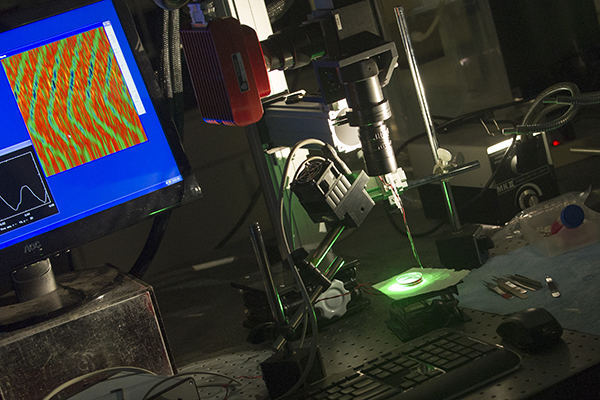
Dr. Noujaim’s laboratory uses specialized equipment to measure the electrical activity of heart muscle cells, including those affected by diabetes.
Among some key findings of the PLOS ONE study:
- Decreasing the expression of GSK3ß in the hearts of the Akita mice reversed cardiac parasympathetic dysfunction. It also increased (improved) parasympathetic response, as measured by the increased high-frequency proportion of heart rate variability.
- Reducing GSK3ß expression also increased activity of IKACH in heart muscle cells of the diabetic mice. The parasympathetic nervous system slows down heart rate through activation of the IKACH potassium current in the cardiac cells. However, Dr. Noujaim said, when GSK3ß is upregulated in response to high glucose levels in the diabetic heart, it causes the suppression of the IKACH current. When IKACH is suppressed, the parasympathetic tone does not reach the heart, thereby allowing the heart-rate accelerating sympathetic nervous system tone to dominate and heart rate variability to decline, he added.
- Collectively, the series of experiments demonstrate that increased GSK3ß activity amplifies cardiac parasympathetic malfunction in type 1 diabetes through regulation of IKACH.
“The data further establish GSK3ß and the GSK3ß signaling pathway as potential therapeutic targets in the treatment and prevention of autonomic dysfunction in diabetic patients,” the study authors conclude.
The research was supported by the Juvenile Diabetes Research Foundation and National Institutes of Health grants.