A unique scientific collaboration that could offer an innovative potential treatment for atrial fibrillation has blossomed within USF Health, thanks to a chance encounter in a hallway, a plain green chalkboard and a most surprising star: the European honeybee.
It represents a convergence of two distinctly different medical mindsets – pharmacology and immunology – and a blend of high-tech bio-engineering with an old-school writing surface. And then there’s the bee, which has pollinated the process in an exciting and novel way.

The result is a newly published paper in the Proceedings of the National Academy of Sciences that details efforts to develop a non-invasive treatment for atrial fibrillation (also referred to as AFIB or AF) by blocking a potassium channel that can go rogue within the heart, leading to a dangerous, irregular and fast rhythm in the atria, the heart’s upper chambers, increasing the risk of blood clots that can travel to the brain and cause a stroke.
The material to create this blocker is a small peptide that has been successfully tested in mice and sheep.
“This peptide was originally isolated in the past from the European honeybee’s venom,” said Sami Noujaim, Ph.D., associate professor in Molecular Pharmacy & Physiology and senior author of the eight-person study that includes lead investigator Bojjibabu Chidipi, Ph.D., a researcher in the USF Health Morsani College of Medicine. “We have demonstrated in tests on small animals that it can block this rogue potassium channel. And by blocking this channel, it was able to eliminate atrial fibrillation.”
That research might well have never progressed to this point had it not been for a pair of fortuitously situated offices. Co-author Michael Teng, Ph.D., an associate professor in the Division of Allergy and Immunology in the College of Medicine, works in an office adjacent to the one occupied by Dr. Noujaim – in spite of their divergent fields.
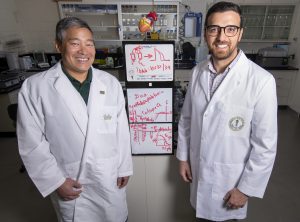
Micheal Teng, PhD, (left) and Sami Noujaim, PhD, have collaborated to study whether a bioengineered peptibody could help treat atrial fibrillation.
“I work in viruses, a completely different area than Sami’s,” said Dr. Teng. “But there’s this green chalkboard hanging on the wall outside our offices – I can see it right now from my desk, in fact. You’d think, ‘Let’s take it down, nobody uses chalkboards anymore.’ But Sami loves this chalkboard. So, we’re neighbors and we talk to each other. And one day, prior to the pandemic, he was trying to figure out a problem.”
Here’s how Dr. Noujaim remembers it unfolding: “I was at the board with Bojji and other members of the lab. We drew the potassium channel on the board. And I was telling them that the drugs currently available for AF are small molecules and have side effects. What if we’re able to actually design our own blocker? And instead of that blocker being a small molecule, what if it was a protein? Because we can design and generate proteins.”
At that moment, Dr. Teng was passing by the group in the hallway en route to his office.
“I go, ‘Hey Mike, I know that in immunology there are ways people have been engineering proteins – can we do this here?’ “ Dr. Noujaim recalled. “Mike said, ‘Absolutely,’ and that’s where things took off.”
Electrical activity is generated by the heart via ion channels of sodium and potassium. They work like resistors and can conduct current. Atrial fibrillation occurs, in part, when a specific type of potassium channel in the heart goes out of whack, and starts passing potassium when it should not.
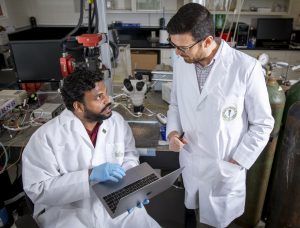
Bojjibabu Chidipi, PhD, (left) talks with Sami Noujaim, PhD, about how a bioengineered peptibody could help treat atrial fibrillation.
“This is where the problem occurs,” Dr. Chidipi said. “Instead of contracting and emptying the blood vessels into the ventricles, and the ventricles contracting and ejecting blood into the circulation, these atria cannot contract because of the atrial fibrillation caused by the rogue potassium current. They just sit there and quiver.”
“When that happens, they cannot completely empty the blood,” Dr. Noujaim added. “And blood does not like to stay stagnant. So there’s a high probability of forming a clot in the atrial chamber. At some point that clot can launch into the circulation and reach the brain, causing a stroke.”
One common form of treatment is to put a person with AFIB on blood thinners. Pharmaceuticals are also utilized to restore normal sinus rhythm of the heart. A more invasive step is called ablation, a procedure in which the trouble spots in the atria are located and corrected via catheters inserted through the groin and advanced to the atria.
“The problem is that there is a high chance the AF will return at some point,” Dr. Noujaim said. “Another alternative is medication. But the problems with the existing medications are two-fold: One, they are not very effective, and two, they may cause other types of arrhythmia. And that is where we came in. We asked ourselves, ‘What would be the best way to restore the normal sinus rhythm with a pharmaceutical, without having other side effects on the heart?’”
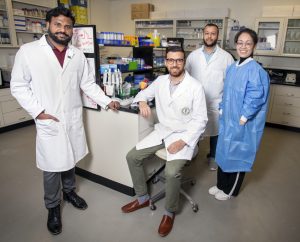
Several members of Dr. Sami Noujaim’s team collaborated on the peptibody research. Pictured (l-r) are Bojjibabu Chidipi, PhD, Dr. Noujaim, Obada Abou-Assali, MS, and Mengmeng Chang, MD, PhD.
Now back to the green chalkboard. The challenge was that the very small peptide, called tertiapin, comprised of 21 amino acids from honeybee venom, doesn’t last long enough to be effective as a blocking agent. It is very short-lived when exposed to air. That led previously to the creation of a synthetic oxidation-resistant version called tertiapinQ. This is what Dr. Noujaim and his team would rely upon in their testing.
But there was still a problem with these peptides breaking down too quickly in the body, whether injected or taken as a pill. So they wondered: Could this peptide be fused with an antibody fragment and give it longer-lasting life to combat AFIB?
“We talked it through and drew on the board for about 15-20 minutes,” Dr. Teng said. “And we came up with this idea of attaching that little peptide onto the stem of an antibody.”
The stem could be hooked onto the peptide, forming a “peptibody.” That concept has been utilized before, but not for treating atrial fibrillation. With this new peptibody AFIB application, a drug could remain in the bloodstream for longer periods of time without breaking down.
“That way you will have a sustained effect of the therapeutics,” Dr. Noujaim said. “Now we have a formulation that does not need to be administered daily– it could be every week or every month. We’re excited to have received a patent for this as well as a nice grant from the National Institutes of Health.”
“So far, there are two peptibodies approved by the FDA and available in the market to treat low blood platelet counts, and for glucose control in type 2 diabetes” Dr. Chidipi added. “We are the first to demonstrate that bioengineered peptibodies could potentially treat cardiac arrhythmia.”
Meanwhile, new collaborators are on board at a cardiovascular center in Spain to work with USF Health in testing it further..
It took collaboration with a bee and a board at USF Health to make it all possible.
— Story by Dave Scheiber for USF Health News; photos by Allison Long, USF Health News.
