At CAMLS, the student teams respond to a series of patient care scenarios including a mock cardiac arrest
Working with a mere 18 months of knowledge and training, second-year USF Pharmacy students made life-or-death decisions in only seconds when they participated in a mock cardiac arrest situation designed to show the different phases of care that pharmacists are involved in for patient care.
The afternoon-long exercise was one of the first virtual patient exercises for the pharmacy students and took place March 18 at USF’s Center for Advanced Medical Learning and Simulation (CAMLS) in downtown Tampa.
The goal of the program was to tie in the students’ communications skills and knowledge of transitions of care with health informatics, said Erini Serag-Bolos, PharmD, assistant professor in the College of Pharmacy.
“This is the first opportunity students have had to put all the tools they’ve learned so far to use,” Dr. Serag-Bolos said “The point is to give them more realistic insight into pharmacists’ various roles across time with a patient.”
The exercise included 10 work stations, most of which played out a patient scenario across time, from the patient first entering the emergency room to follow up care in an outpatient setting. The scenario helped students put into practice the many and varying roles a pharmacist would experience with each patient, including counseling, medication reconciliation, involvement in a cardiac arrest code, pharmaceutical calculations and compatibility, and prescription verification.
“When creating this activity, we wanted to expose them early on and the activity really opened up their eyes to various roles a pharmacist could have in different levels of care and settings – all of course while still having fun with their team,” said Aimon Miranda, PharmD, BCPS, assistant professor.
Working in groups of four to five, students spent five minutes at each station, with some students starting with the emergency room station and others starting at various points in between. By the end, each student completed the entire scenario and pieced all the stations together.
“Students dove into critical points of the patient’s history that they could encounter in their job and that focused on error reduction, patient safety, patient-specific management plans, and health informatics,” Dr. Serag-Bolos said.
In addition, several stations featured standardized patients who acted out these medical scenarios.
“Standardized patients provided a different focus and were good opportunities for the students to practice the patient interview skills they have learned,” Dr. Serag-Bolos said.
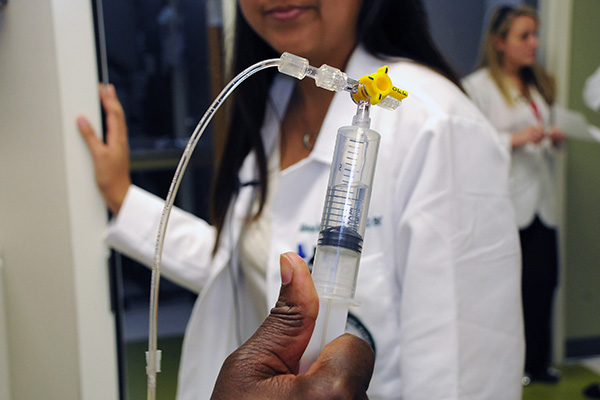
To demonstrate just how unpredictable a day in the life of a pharmacist may be, one of the stations featured a simulator patient mannequin in cardiac arrest that students had to revive. This mannequin could be injected with medications, had a pulse, and was linked to a monitor that could be pre-programmed with certain heart rhythms that were displayed on a monitor.
With a faculty giving orders and providing condition updates of the patient in distress, the students were required to quickly and accurately prepare the medications needed. The patient code provided the most intense situation for the students to use their communication skills, which is the essence of working in teams, Dr. Serag-Bolos said.
“These students haven’t been trained yet for handling emergency code situations, so this definitely got their feet wet,” she said.
“Having no training in advanced cardiac life support, the students had to rely on knowledge and techniques taught in previous semesters,” said Shyam Gelot, PharmD, BCPS, assistant professor. “The students handled themselves very well and confidently during this stressful simulation.”
“Overall, the students did really well given that they had limited information and were expected to think on their feet at each station. In the code station, some students embraced the situation, despite their nerves, and dove in to help their team during the code,” Dr. Miranda said.
And the students agree.
“The ‘code’ scenario was probably my favorite part, but the most stressful,” said Theresa Trindade, a second-year pharmacy student. “The way I can describe this exercise succinctly is that it was a challenge. It forced us to think on our feet.”
At the end of the exercise, the students met with faculty in a nearby conference room to debrief on how well they performed, their reactions to the emergency, and the success, or failure, of communicating with their peers in order to benefit the patient.
“I thought the exercise was a great hands-on learning experience and was a good opportunity to apply, under a simulated clinical setting, the information I am learning in my lectures and in my readings,” said Phillip Bonet, also a second-year student.
“The most challenging aspect was the patient rooms because we had to figure out the level of care and what was going on with the patient,” Trindade added. “I think my group excelled in certain areas. For example, one of our group members who did the counseling for insulin did a really good job. We were less sure in the patient rooms where we had to make recommendations. I think this was a great learning exercise and showed us all the roles a pharmacist plays in patient care.”
Housed in the CAMLS Virtual Patient Care Center and both virtual inpatient and outpatient pharmacies, the venue provided a state-of-the-art backdrop for the transitions of care exercise. This facility provides an outstanding setting for the interprofessional program that pharmacy students take part in to hone communications skills with students from multiple educational tracks (medicine, nursing, pharmacy, and physical therapy). These exercises offer more realistic views of how interprofessional healthcare teams care for patients, especially those who require multiple visits. To ensure optimal care and reduce hospital readmissions, patients’ therapeutic plans need to be reassessed as their conditions change. All of these reasons reinforce the fact that students should train in teams because they will likely work in teams throughout their careers.
The concept is part of USF College of Pharmacy’s innovative curriculum.
“I decided to attend USF COP because, from the various schools I was exploring, it seemed to me that USF had the most progressive program and would prepare me well for my future in the profession,” Bonet said. “The simulation activity at CAMLS as a second year student is a great example of this.”
Story by Sarah A. Worth, USF Health Office of Communications
Photos and video by Allyn DiVito, USF Health Information Systems