USF Health’s Dr. Kami Kim probes the epigenetics of two global parasitic infections, malaria and toxoplasmosis
While an undergraduate at Harvard University, Kami Kim, MD, participated in a research thesis project exploring leukemia’s resistance to chemotherapy and the effectiveness of combination drugs in combatting it. While she was excited to help figure out (and publish) a mechanism, she recalls that she signed on for this laboratory research primarily “to help in get into medical school.”
Her interest in research intensified in medical school in early 1980s at the beginning of the domestic AIDS era, about the same time tuberculosis cases were exploding and malaria, once considered virtually eliminated as a major public health threat, began to re-emerge globally.
“It was clear that there was much to be done in infectious diseases research — a lot of interesting problems that needed to be solved,” said Dr. Kim, who joined the USF Health Morsani College of Medicine last year as a professor in the Department of Internal Medicine’s Division of Infectious Disease and International Medicine.

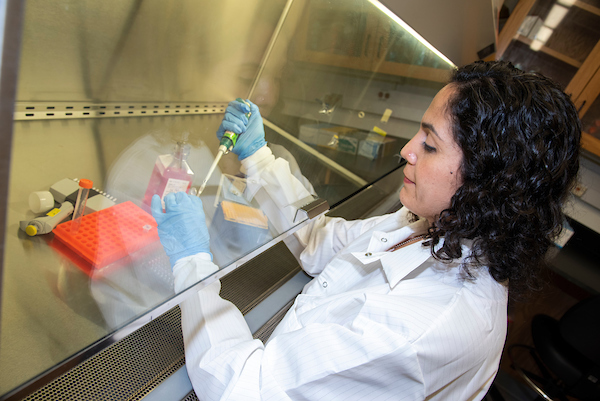
Kami Kim, MD, a USF Health professor of infectious disease, with her multidisciplinary laboratory research team, which includes expertise from the medicine, public health, mathematics and statistics
![]() Undergraduate laboratory work that sparked a lifelong passion for research
Undergraduate laboratory work that sparked a lifelong passion for research
Basic science and clinical infectious diseases expertise
After clinical training as an infectious diseases fellow at the University of California San Francisco (UCSF) – and witnessing firsthand the devastating consequences of acquired immunodeficiency syndrome – Dr. Kim returned to laboratory research, with an emphasis on parasitic infectious diseases. Meanwhile, she continued to see patients as an attending academic physician at some of the nation’s best hospitals in San Francisco and New York City.
That blend of rigorous clinical and basic science expertise makes Dr. Kim one of the first of several high-profile, energetic recruits who will help take USF Health’s global infectious disease research to the next level.
Dr. Kim came to USF Health in November 2017 from Albert Einstein College of Medicine in New York City, where she was a professor of medicine, microbiology and immunology, and pathology. In addition to her laboratory research at USF, she consults monthly on infectious diseases cases at Tampa General Hospital. At Einstein, she directed the infectious diseases section of the Center for Epigenomics and helped launch and led the National Institutes of Health-funded Geographic Medicine and Emerging Infections Training Program, which supports interdisciplinary training in translational research for pre-doctoral students, post-doctoral research fellows and clinical fellows.
Seeking solutions to life-threatening global parasitic diseases
Dr. Kim’s USF Health research team, working out of a laboratory in the university’s research park, focuses on two major areas — malaria and toxoplasmosis. The world’s most dangerous parasitic disease, malaria claims more than 2 million victims and 445,000 deaths yearly, primarily in sub-Saharan Africa. Toxoplasmosis, often asymptomatic, can be life-threatening to babies born to women infected during pregnancy and people with weakened immune systems.
- Toxoplasmosis project: Combining advanced techniques from genetics, cell biology and proteomics, the researchers investigate the ways that epigenetics – the interface of genetics and environmental factors – regulate development of chronic infection by the cat-borne gondii parasite. They seek to understand how this pervasive parasite switches back and forth between a rapidly dividing acute stage destructive to healthy tissue (tachyzoite) and a chronic, or dormant, stage, where bradyzoite forms within pseudocysts remain invisible to the immune system. Dr. Kim collaborates with other leading Toxoplasma experts: Distinguished USF Health Professor Michael White, PhD, a long-time colleague, as well as investigators at Indiana University, Pennsylvania State University and Albert Einstein College of Medicine.
- Malaria project: In the hot, wet regions of Africa, mosquitoes are ubiquitous and children exposed to malaria from birth may contract the infection several time a year. The overwhelming majority of clinical cases are uncomplicated, with flu-like symptoms of fever and malaise that typically resolve. Researchers are trying to determine why a small percentage of individuals, in particular certain children, are more likely to develop severe malaria with coma and death (cerebral malaria) or long-term neurological complications such as seizures and cognitive and behavioral problems. In particular, the USF team is assessing specific biomarkers, or genetic predispositions, and parasite or host factors that may help predict disease development or its outcomes.
![]() Dr. Kim discusses research correlating HIV co-infection with cerebral malaria.
Dr. Kim discusses research correlating HIV co-infection with cerebral malaria.
Both research initiatives harness the latest genomic technology to better understand how immunity works within the framework of host-parasite interactions – all with the aim of devising better or first-time treatments.
Valuable insights into cerebral malaria, future therapies
With collaborators from the Blantyre Malaria Project, based in Malawi, Africa, Dr. Kim published a high-profile paper in mBIO in 2015 reporting for the first time that children co-infected with HIV were much more likely than those who were not to die from severe malaria. Autopsies of the children who died from cerebral malaria indicated that those with HIV had brain blood vessels more clogged with white blood cells and platelets than those of children with malaria alone. HIV appeared to rev up brain inflammation that could lead to death.
In another study, published in Cell Host & Microbe in 2017, Dr. Kim and colleagues used neuroimaging, parasite transcript profiling and laboratory blood profiles to develop machine-learning models of malarial retinopathy and brain swelling. The researchers found that the interaction of high parasite biomass, low platelet levels and certain parasite protein variants that bind to the endothelial protein C receptor (EPCR) play a pivotal role in fatal cases of malaria. Their findings added strength to the rationale that anti-inflammatory and anticoagulant treatments counteracting the breakdown of endothelium may benefit those with severe malaria.
“We still don’t entirely know why some of these kids get super sick and have complications requiring hospitalization,” Dr. Kim said. “If we could figure that out we could save lives, reduce complications and use limited healthcare dollars more effectively in these under-resourced countries.”
The “Goldilocks” theory of immunity
When it comes to infectious diseases, too much of a good thing may make you sick. Dr. Kim calls it the “Goldilocks” theory of immunity – not too much (overactive immune system) and not too little (under-responsive immune system).
For instance, “for someone with malaria the right amount of immunity might not be just the right amount if they already also have tuberculosis,” Dr. Kim said. “What we’re realizing now with the human immune response to parasites or other foreign invaders (pathogens) is that you have to get the balance just right, so you get rid of the pathogen without damaging the human host.”
Otherwise, she added, even after the pathogen is eliminated, long-term complications like a damaging autoimmune inflammatory condition may linger.
Rigorously studying the dynamics of host-parasite interaction – including how parasites hijack the epigenome, which adjusts specific genes in response to signals from the outside world such as diet and stress — is critical to bridging the gap between discovery and effective treatments for different subgroups of infected patients.
“Both the pathogen and the infected host are duking it out to see which one wins, so figuring out what’s happening on both sides is really important to understanding immunity – how our body fights off disease,” Dr. Kim said. “Using genomic information to tell us who’s most susceptible to certain conditions will likely help us to tailor therapies to the individual, or perhaps to know who needs to be vaccinated.”

Dr. Kim with Li-Min Ting, PhD, an assistant professor in the Department of Internal Medicine’s Division of Infectious Disease
![]() Striking the right balance of immunity
Striking the right balance of immunity
Potential applications for other diseases
Within their complex life cycles, both malaria and toxoplasma parasites have dormant forms that the human immune system can’t identify and kill, and antimicrobial drugs can’t touch. For malaria, this silent form lurks in the liver. For Toxoplasma, cysts can settle quietly into the infected person’s brain and muscle tissue without replicating, sometimes for years, until weakened immunity reactivates the disease.
Dr. Kim and other researchers continue to look for new ways to combat chronic infection by parasites.
“Normally when treating a disease you think of killing the form that makes a person clinically symptomatic,” she said, “but with both malaria and Toxoplasma if you can kill the biologically silent form, which is absolutely essential for the disease to continue, you’re accomplishing the same thing.”
Although Dr. Kim’s group targets specific problems underlying malaria and toxoplasmosis, such immune research may have broad applications for understanding and treating other conditions. For instance, atherosclerosis has been linked to the release of molecules from the immune system that can cause inflammation, blood vessel injury and plaque instability leading to heart attacks and stroke.
“Even though drug companies, because of financial return on investment, aren’t necessarily willing to invest in research on malaria host factors,” Dr. Kim said, “they are really interested in stroke and cardiovascular disease. And the big players in the kind of inflammation seen in these two major diseases are platelets and monocytes” – the same inflammatory culprits implicated in cerebral malaria.
While more research is needed, perhaps statin and antiplatelet drugs already approved for another indication could be effective in helping combat malaria,” she said. “It’s entirely possible by better understanding what’s a good immune response to malaria in one situation and bad in another will lead to insights that can be used to develop treatments for other diseases, or insight into what’s protective in another disease.”
Pursuing new approaches to outsmart elusive pathogens
Dr. Kim received her MD degree from the Columbia College of Physicians and Surgeons in New York City. She completed her residency in medicine at Columbia-Presbyterian Medical Center, a clinical fellowship in infectious diseases at UC San Francisco, and two postdoctoral research fellowships – one in parasitology at San Francisco General Hospital and a second in microbiology and immunology at Stanford University.
Dr. Kim is a fellow of the Infectious Diseases Society of America and the American Academy of Microbiology. She is also an elected member of American Society for Clinical Investigation and the Association of American Physicians, national honor societies for physician-scientists. A recipient of the Burroughs Wellcome Fund (BWF) New Investigator Award in Molecular Parasitology early in her career, she has served on the BWF Postdoctoral Research Enrichment Program’s scientific advisory board since 2014. She is a member of the NIH Pathogenic Eukaryotes Study Section.
Throughout much of her career, Dr. Kim’s research has been funded by the National Institute of Allergy and Infectious Diseases. She holds several patents, and was one of the first investigators to develop techniques to genetically manipulate T. gondii. She is the co-editor and currently preparing the third edition of Toxoplasma gondii, the Model Apicomplexan: Perspectives and Methods, a textbook widely considered the seminal source for scientists and physicians working with this parasite.
Dr. Kim said she was attracted to USF because of the university’s upward national trajectory and USF Health leadership’s commitment to building translational research and pursuing innovative approaches and excellence in all its academic missions. She is a member of the USF-wide Genomics Program.
“I enjoy being part of a USF clinical community that excels in the treatment of infectious diseases and working with physicians and scientists who do parasitology research,” she said. “You constantly have to think outside the box and come up with clever strategies – because we’re dealing with pathogens that do not behave like they are supposed to.”
![]() Toxplasma parasite strategy for survival
Toxplasma parasite strategy for survival

Dr. Kim, one of the first investigators to develop techniques to genetically manipulate Toxoplasma gondii, co-edits a textbook widely considered the seminal source for scientists and physicians working with this parasite.
Some things you might not know about Dr. Kim
- Korean was her first language, and she also speaks Spanish.
- She enjoys food, arts and crafts, and travel. Countries she has visited include Korea, Malawi, South Africa, France, Japan, and Brazil.
- Kim is married to Thomas McDonald, MD, USF Health professor of cardiovascular sciences and director of the new Cardiogenetics Clinic. They have two sons who are both mathematicians, one in a mathematics PhD program and the other in college. They met in the cardiac intensive care unit at Columbia Presbyterian Medical Center when Dr. McDonald was a resident and Dr. Kim was rounding as a medical student.

Dr. Kim’s career as an infectious disease physician-scientist bridges basic research and clinical practice.
-Video and photos by Torie M. Doll, USF Health Communications and Marketing