]]>
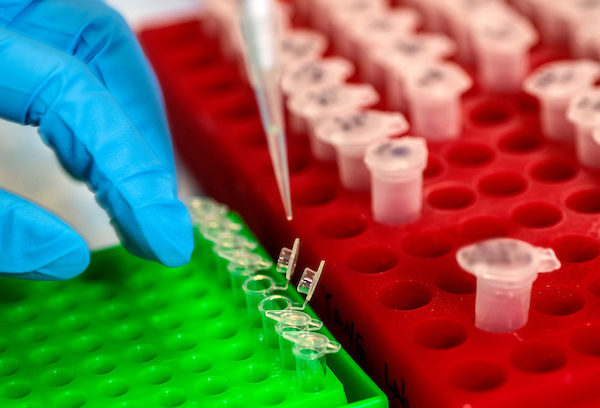
Targeting the gene Foxo1 may offer an early treatment approach for hereditary lymphedema, USF Health preclinical study reports
Principal investigator Ying Yang, PhD, is an assistant professor of molecular pharmacology and physiology in the USF Health Morsani College of Medicine and a member of the college’s Heart Institute. | Photo by Allison Long, USF Health Communications
Tampa, FL (Aug. 9, 2021) — A University of South Florida (USF Health) preclinical study unexpectedly identified the gene Foxo1 as a potential treatment target for hereditary lymphedema. The research, published July 15 in The Journal of Clinical Investigation, was done with colleagues from Tulane University and the University of Missouri.
Lymphedema — a chronic condition in which lymphatic (lymph) fluid accumulates in soft tissue under the skin, usually in the arms and legs — causes minor to painfully disfiguring swelling. Primary, or hereditary, lymphedema is rare, present at birth and caused in part by genetic mutations that regulate normal lymphatic valve development. Secondary, or acquired, lymphedema is caused by damage to the lymphatic system from surgery, radiation therapy, trauma, or parasitic infection. In the U.S., lymphedema most commonly affects breast cancer patients, with prevalence ranging from 10 to 40% after lymph node removal and radiation therapy.
While lymphedema can be managed with massage and compression garments, no treatment exists to address its underlying cause: the build-up of fluid that eventually backs up in the lymph system like an overflowing sink with a blocked drain. This stagnant lymph triggers an inflammatory response that can induce connective and fatty tissue to form and harden the skin, restricting movement and increasing the risk of recurrent infections.
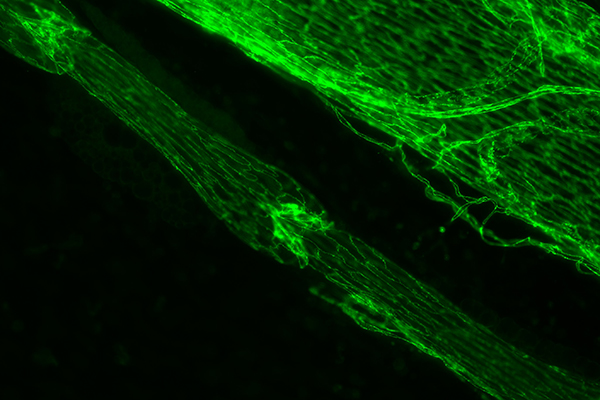
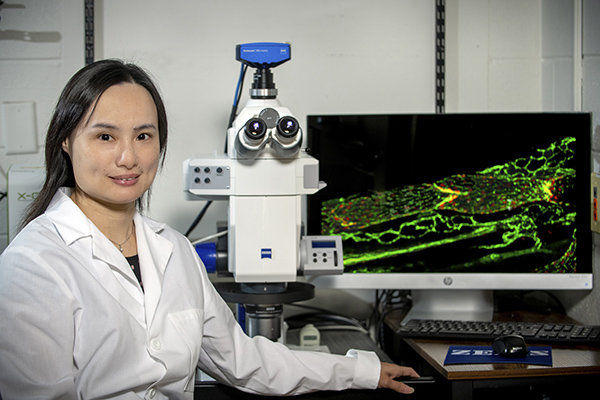
Green immunostained image of a lymphatic vessel with one valve in the center and another in the top left corner. To the upper right of the lymph vessel is a large vein. | Photo courtesy of Joshua Scallan, PhD.
“The later fibrosis stage of lymphedema cannot be massaged away,†said study principal investigator Ying Yang, PhD, assistant professor of molecular pharmacology and physiology at the USF Health Morsani College of Medicine. “Targeting lymph valves early in the disease is one critical aspect in identifying an effective treatment for lymphedema. If the disease progresses too far, it’s difficult to reverse.â€
Valve loss or dysfunction that disrupts the flow of lymph fluid is strongly associated with lymphedema in patients. But no one has discovered whether new valves can be grown or if defective ones can be fixed.
The USF Health-led study shows that both are possible.
Dr. Yang’s group hypothesized that the protein encoded by the gene Foxo1 plays a key role in lymph valve formation based on an earlier USF Health discovery of cell signaling processes controlling formation of lymph valves. The researchers showed that deleting a single gene — lymphatic vessel-specific Foxo1 — promoted the growth of markedly more valves in both young postnatal mice and adult mice than in control littermates without Foxo1 deletion. Furthermore, deleting Foxo1 in a mouse model mimicking human lymphedema-distichiasis syndrome fully restored the both the number of valves and valve function.
“It was exciting to see that Foxo1 is the only gene so far reported that, when deleted, induces more lymphatic valves to form, instead of inhibiting valve growth,†said Dr. Yang, a member of the USF Health Heart Institute. “We actually reversed valve loss and repaired the structure and function of defective valves in a genetic mutation model of lymphedema…That type of discovery makes a study clinically relevant.â€
The lymphatic circulatory system – a parallel of the blood vessel circulatory system – helps maintain healthy fluid balance in the body by collecting and controlling the flow of extra lymph fluid that leaks from tissue. This complex network propels watery lymph fluid carrying proteins, nutrients and toxin-destroying immune cells through the body in one direction before returning the fluid to circulating blood. Small valves inside lymph vessels open and close in response to force exerted by the lymph fluid, moving it forward and preventing backward flow into tissues.
Dr. Yang in her lab where she researches lymphedema, which in the U.S. most commonly occurs in some breast cancer patients after lymph node removal and radiation therapy. Some of the research is light sensitive and must be conducted in near darkness. | Photo by Allison Long, USF Health Communications
Among the key study findings:
- The protein FOXO1 (encoded by gene Foxo1) inhibits lymph valves from developing by suppressing many genes, which collectively contribute to the multi-step process of making a mature valve. FOXO1 behaves like a brake on a set of valve-forming genes, Dr. Yang said. “Once the brake is removed, all those genes can now be expressed so that new valves can successfully grow.â€
- Inactivation (knockout) of Foxo1 in lymphatic endothelial cells (LEC) of young postnatal mice promoted valve formation at multiple stages. Likewise, deleting LEC-specific Foxo1 in adult mice also increased valve formation, compared to control mice without the gene knockout.
- A mouse model of lymphedema-distichiasis syndrome had 50% fewer lymphatic valves and the remaining valves closed abnormally and exhibited fluid backflow. But when Foxo1 was deleted, the number of valves increased to the same levels as those in healthy control mice and the structure of defective valves was restored to normal. Further analysis showed that the loss of Foxo1 also significantly improved valve function in this mouse model of human primary lymphedema disease.
This study was supported by grants from the National Heart, Lung, and Blood Institute, a part of the National Institutes of Health. USF Health’s Joshua Scallan, PhD, was the lead author.
]]>
]]>
Preclinical study shows microRNA approach inhibited re-narrowing while healing vessels
Tampa, FL (Aug. 18, 2014) — A new therapy developed by researchers at the University of South Florida (USF) Morsani College of Medicine and Columbia University Medical Center (CUMC) may help reduce the life-threatening complications of interventional cardiovascular disease treatment.
The researchers demonstrated in a rat model that the novel molecular therapy could selectively inhibit blood vessel re-narrowing and simultaneously promote vessel healing following a medical procedure using a balloon catheter to open narrowed or blocked arteries.
Their preclinical study was published in Sept. 2, 2014 in the Journal of Clinical Investigation.

Hana Totary-Jain, PhD, assistant professor of molecular pharmacology and physiology at the USF Health Morsani College of Medicine, was principal investigator for the study.
“This innovative microRNA-based strategy can be used to combine anti-proliferative and pro-healing mechanisms for improved repair of coronary arteries,†said the study’s principal investigator Hana Totary-Jain, PhD, assistant professor of molecular pharmacology and physiology at the USF Health Morsani College of Medicine, who came to USF Health from CUMC last year to join the USF Health Heart Institute.
“The most significant finding of our study is that for the first time we were able to achieve in one fell swoop both the inhibition of cells responsible for re-narrowing of the vessel, and preserving the ‘good’ endothelial cells that protect against thrombosis,†said lead author Gaetano Santulli, MD, PhD, a cardiologist working at CUMC’s College of Physicians & Surgeons.
Angioplasty, the world’s most common medical procedure, opens a narrowed or blocked artery by inserting a small balloon into the blood vessel. If the artery is blocked, a tiny wire-mesh tube, known as a stent, is mounted on the end of the balloon to leave in the vessel when the balloon is removed. The stent holds the artery open and maintains blood flow after angioplasty clears the vessel of fatty deposits. Physicians performed 560,500 angioplasties in the United States in 2011, according to a recent report by the Agency for Healthcare Research and Quality,and, Dr. Santulli said, 70 to 90 percent of all angioplasty patients receive one or more stents.
Together, angioplasty and stenting have helped advance the field of interventional cardiology and save lives.
Drug-eluting stents, first approved for use in the United States in 2003, dramatically reduced rates of restenosis compared to earlier bare metal stents. Medications coating these stents thwart the development of scar tissue causing the treated coronary artery to re-narrow, a complication often requiring another procedure.
While the drug-eluting stent overcame the obstacle of restenosis, research eventually showed that the medications released by the device were not specific — meaning they failed to discriminate between destructive and beneficial cells. The drugs blocked proliferation and migration of vascular smooth muscle cells leading to artery re-narrowing, but they also blocked regrowth of endothelial cells indispensable to healing blood vessel walls disrupted by stent implantation.
Formation of blood clots several months or even years after initial implantation remains a severe, though rare, increased risk associated with the lack of endothelium covering the treated vessel. This risk for late stent clotting, or thrombosis, requires patients to stay on prolonged dual antiplatelet therapy to help prevent life-threatening heart attacks — but not without increasing the odds of major bleeding.

Gaetano Santulli, MD, PhD, of Columbia University Medical Center, was lead author.
With this history in mind, researchers at USF and CUMC harnessed the intrinsic power of microRNAs — master regulators of gene expression affecting many biological processes including cell proliferation — to create a more selective therapy.
Their goal was to inhibit blood vessel re-narrowing and, at the same time, allow endothelial cells to regrow and heal the vessel. They tested the experimental therapy in a rat model of balloon angioplasty injury, and discovered it worked.
Among the findings:
–         As soon as two weeks following arterial injury induced by balloon angioplasty, the injured arteries in the rats receiving microRNA-based therapy were 80 percent covered with new endothelium. In the group receiving a molecular therapy that mimicked drug-eluting stents, endothelial cell coverage remained below 30 percent even after one month. “The difference was quite amazing,†Dr. Totary-Jain said.
–Â Â Â Â Â Â Â Â Â Measures of blood clotting in the microRNA-based therapy group at two weeks post-injury were reduced to the same levels as in the uninjured control animals.
–         In addition to helping protect against thrombosis-associated clotting, the endothelial cells restored in the treated group appeared to work as well in helping dilate blood vessels as endothelial cells in the vessels of the healthy, untreated control group. “From a clinical point of view, reduced thrombosis and functional vascular responses represent the most promising aspects of the whole study,†Dr. Santulli said.

Dr. Totary-Jain works with Jamie Chilton, PhD, one of the study’s co-authors.
More studies are needed, including implanting stents to test the therapy in other models of atherosclerosis and diabetes.
“This is just the first step, but we are working on tailoring the strategy to be more effective,†Dr. Totary-Jain said. “The combination of this selective therapy with a better stent platform and biodegradable polymer has the potential to revolutionize the future of vascular interventional medicine.â€
The USF/CUMC study was supported by the American Heart Association and the National Institutes of Health/National Heart, Lung and Blood Institute.
Article citation: Gaetano Santulli, Anetta Wronska, Kunihiro Uryu, Thomas G. Diacovo, Melanie Gao, Steven O. Marx, Jan Kitajewski, Jamie M. Chilton, Kemal Marc Akat, Thomas Tuschl, Andrew R. Marks, Hana Totary-Jain; “A selective microRNA-based strategy inhibits restenosis while preserving endothelial function;â€Journal of Clinical Investigation: 2014;124 (9):4102-4114. DOI: 10.1172/JCI76069.
-USF Health-
USF Health’s mission is to envision and implement the future of health. It is the partnership of the USF Health Morsani College of Medicine, the College of Nursing, the College of Public Health, the College of Pharmacy, the School of Biomedical Sciences and the School of Physical Therapy and Rehabilitation Sciences; and the USF Physician’s Group. The University of South Florida is a Top 50 research university in total research expenditures among both public and private institutions nationwide, according to the National Science Foundation. For more information, visit www.health.usf.edu
]]>
]]>
A Dana-Farber/Boston Children’s and VA Hospital/University of South Florida team created the antiviral therapy, which harnesses the power of stapled peptide and nanoparticle technologies to thwart the respiratory virus
Boston, MA, and Tampa, FL (April, 17, 2014) — New therapies are needed to prevent and treat respiratory syncytial virus (RSV) – a potentially lethal respiratory infection that can severely affect infants, young children and the elderly.
Despite a wide range of anti-RSV efforts, there are no vaccines or drugs on the market to effectively prevent or treat the infection.
Now researchers at the Dana-Farber/Boston Children’s Cancer and Blood Disorders Center and Harvard Medical School in Boston, MA, and the James A. Haley VA Hospital and the University of South Florida (USF) in Tampa, FL, have developed novel double-stapled peptides that inhibit RSV in cells and in mice. The team also showed that this peptide’s capacity to block infection was significantly boosted when delivered to the lungs by miniscule, biodegradable particles known as nanoparticles.
The team’s findings are reported online today in The Journal of Clinical Investigation.Â

Shyam Mohapatra, PhD, leads the VA/University of South Florida research team with expertise in nanoparticle technology. He holds a test tube of nanoparticle solution.
RSV employs a fusion protein with a helical structure to enable the virus to bind to and penetrate epithelial cells lining the nose and lungs.
The Dana-Farber/Boston Children’s/Harvard laboratory led by co-senior author Loren Walensky, MD, PhD, used their chemical strategy known as hydrocarbon stapling to make “double-stapled†RSV peptides. Stapling helps the peptides retain their natural helical shape and resist degradation by the body’s enzymes while disrupting the fusion process needed for RSV to infect host cells.
The VA/USF group led by co-senior author Shyam Mohapatra, PhD, tested these double-stapled peptides, alone and in combination with propriety nanoparticles, in mice to demonstrate significant inhibition of RSV infection.
“This is an exciting advance in the fight against respiratory syncytial virus infection,†said Dr. Mohapatra, director of the USF Nanomedicine Research Center and the USF Health Morsani College of Medicine’s Division of Translational Medicine, and a research career scientist at James A. Haley VA Hospital.
“We found that double-stapled peptide interference targeting the virus fusion protein can be administered in the form of a nasal drop or spray. The treatment suppressed viral entry and reproduction, including spread from nose to lungs, providing substantial protection from infection when administered several days before viral exposure.â€
“Designing therapeutic peptides based on a virus’ very own fusion apparatus was previously exploited to block HIV-1 infection, but this class of drugs was severely limited by the pharmacologic liabilities of peptides in general, including loss of bioactive structure and rapid digestion in the body,†said Dr. Walensky, associate professor of pediatrics at Harvard Medical School, pediatric hematologist/oncologist at Dana-Farber/Boston Children’s and principal investigator in Dana-Farber’s Linde Program in Cancer Chemical Biology.
“Peptide stapling restores the natural helical shape, which also inhibits proteolysis, providing a new opportunity to take advantage of a well-validated mechanism of action to thwart viruses like RSV that otherwise lack drugs for preventing or treating infection.â€

Loren Walensky, MD, PhD, leads the Dana-Farber/Boston Children’s/Harvard laboratory with expertise in stapled peptide technology. The screen image shows the chemical structure of a stapled peptide, with the arrow pointing to the hydrocarbon staple (in yellow).
Dr. Mohapatra and his team developed nose drops containing the Walensky laboratory’s double-stapled peptides after combining them with TransGenex’s chitosan nanoparticles that stick to mucous-producing cells lining the lungs.
First, the researchers treated mice intranasally with stapled peptide nose drops, both before and during infection with RSV. The treated mice showed significantly lower levels of virus in the nose and lungs, and less airway inflammation, compared to untreated mice.
Then, double-stapled peptides encapsulated in nanoparticles were delivered to the lungs via the trachea to test whether the combination could further increase the effectiveness of this experimental therapy. The nanoparticle preparation markedly improved delivery of the peptides to the lungs, and the combination worked better and longer in preventing RSV pneumonia than the double-stapled peptide alone.
The researchers say to the best of their knowledge this preclinical study is the first to combine peptide stapling and nanoparticle technologies to maximize the delivery, persistence, and effectiveness of an antiviral therapy.
RSV is the most common virus causing lung and airway infections in infants and young children. Most have had this infection by age 2, and it can be especially serious, even deadly, in high-risk groups, such as babies born prematurely and those whose immune systems do not work well. The virus hospitalizes thousands of infants each year for pneumonia or brochiolitis and has been associated with a significantly greater risk of developing asthma later in life. The elderly are also at high risk of complications from RSV infection.
“This is a new way forward in the development of strategies to prevent RSV infection,†said Terrence Dermody, MD, the Dorothy Overall Wells professor of pediatrics and director of the Division of Pediatric Infectious Diseases at Vanderbilt University School of Medicine, who was not involved with the research. “The authors are to be complimented on the clever design, interdisciplinary approach and extension from cell-culture experiments to animal studies. I am particularly excited about the possible application of this technology to other viruses.â€
The study was supported in part by grants from the National Institutes of Health, Research Career Scientist and VA Merit Review Awards from the U.S. Department of Veterans Affairs, and a Burroughs Wellcome Fund Career Award.
Article citation:
Gregory H. Bird, Sandhya Boyapalle,Terianne Wong, Kwadwo Opoku-Nsiah, Raminder Bedi, W. Christian Crannell, Alisa F. Perry, Huy Nguyen, Vivianna Sampayo,  Ankita Devareddy, Subhra Mohapatra,  Shyam S. Mohapatra and Loren D. Walensky, “Mucousal delivery of a double-stapled RSV peptide prevents nasopulmonary infection,â€Â  Journal of Clinical Investigation, 2014;124(5): doi:10.1172/JCI71856.
About Dana-Farber/Boston Children’s Cancer and Blood Disorders Center
Dana-Farber/Boston Children’s Cancer and Blood Disorders Center brings together two internationally known research and teaching institutions that have provided comprehensive care for pediatric oncology and hematology patients since 1947. The Harvard Medical School affiliates share a clinical staff that delivers inpatient care at Boston Children’s Hospital and outpatient care at the Dana-Farber Cancer Institute’s Jimmy Fund Clinic. Dana-Farber/Boston Children’s brings the results of its pioneering research and clinical trials to patients’ bedsides through five clinical centers: the Blood Disorders Center, the Brain Tumor Center, the Hematologic Malignancies Center, the Solid Tumors Center, and the Stem Cell Transplant Center.
About USF Health
USF Health’s mission is to envision and implement the future of health. It is the partnership of the USF Health Morsani College of Medicine, the College of Nursing, the College of Public Health, the College of Pharmacy, the School of Biomedical Sciences and the School of Physical Therapy and Rehabilitation Sciences; and the USF Physician’s Group. The University of South Florida is a Top 50 research university in total research expenditures among both public and private institutions nationwide, according to the National Science Foundation. For more information, visit www.health.usf.edu
Media contacts:
Anne DeLotto Baier, USF Health Communications, University of South Florida
(813) 974-3303 or abaier@health.usf.edu
Irene Sege, Dana-Farber/Boston Children’s Cancer and Blood Disorders Center
617-919-7379 or irene.sege@childrens.harvard.edu
]]>