Coronavirus and Health Equity- Again This (Too) Is Predictable
by Kevin B. Sneed, PharmD, FNAP, FNPHA
The current COVID-19 pandemic represents the most unprecedented health event to occur across the globe in over a generation. Initial indicators of the severity of the emerging pandemic were revealed when the Wuhan, Hubei province, China ceased all daily and economic activity within their region in January 2020 to attempt to contain the spread of a novel coronavirus, now identified as SARS-CoV-2 (WHO 2020). Human infections were quickly detected in dozens of countries outside of China, with the first confirmed identification inside of the United States on January 20, 2020 ( N Engl J Med 2020; 382:929-936). The spread across the United States has been dramatic; at the time of this writing there are 321,762 confirmed cases in the United States, and 1,237,420 worldwide (Johns Hopkins University Covid-19 map). The most affected state has been New York, with 114,996 cases, and 3,568 deaths. New York City has the highest infection and death counts, with 63,307 cases, and 2,254 deaths. For the past two weeks, New York and New York City have been the epicenter of SARS-CoV-2 in the United States. It makes geographical sense that New Jersey has the second highest infection and death counts. According to the University of Washington Institute for Health Metrics and Evaluation (IHME), peak utilization of hospital resources is expected to occur in New York by April 8-9 (Fig 1), with nationwide peak resource utilization expected to occur by April 15 (Fig 2).
Figure 1 – NY state data. Obtained 04/05/2020 at www.covid19.healthdata.org
Figure 2 – USA data. Obtained 04/05/2020 at www.covid19.healthdata.org
While the most attention to the COVID-19 outbreak has been focused on Washington state (early outbreaks) and New York (most severe outbreaks), newly emerging hotspots in Michigan, Louisiana, and Illinois begin to reveal another pattern. The outbreaks are focused in densely populated cities, with the most affected areas concentrated in counties and neighborhoods with higher racial and ethnic populations. This is particularly concerning as the highest rates of chronic illnesses, and particularly cardiovascular chronic illnesses, are also concentrated in these areas. It has been become widely accepted that Covid-positive patients with comorbid conditions such as hypertension, diabetes, and diagnosed cardiovascular disease also experienced the highest mortality rates (Wu Z, et al JAMA. doi:10.1001/jama.2020.2648). These locations likely represent patients that are dependent on public transportation, may be classified as essential workers, and reside in socially dense housing (Associated Press, Wire Service Content-April 3, 2020, at 4:25 p.m.). Population density, while not the final factor, must be considered and identified as a significant factor for spread of SARS-CoV-2. And people of color and identified ethnic groups may disproportionately represent the largest burden to the healthcare systems.
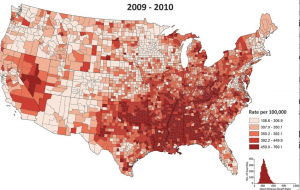
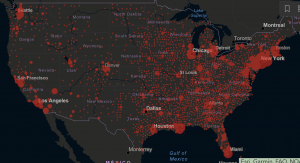
The New Orleans SARS-CoV-2 outbreak has particular significance, given the city’s demographics and demonstrable social activities. Epidemiology experts at both Tulane University and Louisiana State University have stated that recent Mardi Gras activities, which concluded February 25, likely contributed to the rampant virus spread in Louisiana. The more concerning component of the spread is the well-established cardiovascular disease status of the state, and in particular in New Orleans. The southern corridor of cardiovascular disease is especially concerning given the evident morbidity and mortality associated with patients affected by SARS-CoV-2. Figure 3 shows the well-established cardiovascular burden in the southern United States, and almost directly coincides with the geographical locations of diagnosed SARS-CoV-2 cases (Figure 4). While I’m not suggesting that existent cardiovascular disease is the cause of the Covid spread, it does provide a window into the greatest probable mortalities that may be associated with a SARS-CoV-2 outbreak in these overlapping areas.
Figure 3 – Cardiovascular Disease prevalence- adapted from American Heart Association data – 04/03/2020
Figure 4 – Johns Hopkins University Covid-19 map – confirmed cases – accessed 04/05/2020
The question of placement of needed medical resources to combat the expected peaks of SARS-CoV-2 cases requiring hospitalization have been occurring for weeks. There is the growing question of the health equity (and in some cases inequity) of supplied medical resources in those areas with a high prevalence of racial and ethnic citizens, and those on the lower socioeconomic strata. Public health officials across the country have likely been the best equipped individuals to guide the discussion of where and when medical resources should be dispatched. The negative economic impact caused by the spread of the virus has been devastating not only to the country as a whole, but those communities and individuals that depend on service-focused employment to drive the economic engine of the United States. I have every confidence that the medical research community will eventually find effective tools to combat coronavirus by creation of vaccines, medications, and more effective testing and surveillance. The connections between the previously referenced JAMA article (wu Z et al) and Figures 3 and 4 strongly point to who is going to most likely be impacted by this pandemic in our country, and even more importantly where they are located. As each anticipated hotspot prepares for very probable significant impacts to their healthcare systems, we should also have foresight to more aggressively address the inequities in healthcare that exist within our country. Each and every individual that positively contributes to our society must be provided the opportunity to maintain reasonably good health in order to have the capability to pursue life, liberty, and happiness in this great United States of America. Data provides the best pathway to achieving this end.
Kevin B. Sneed, PharmD, FNAP, FNPHA
Senior Associate Vice-President, USF Health
Dean and Professor, Taneja College of Pharmacy
University of South Florida