Several years ago, I experienced a patient encounter that signaled to me that the future of mobile health technologies is primed for democratization by patients. As dean of the USF College of Pharmacy, a member of USF Health, I still prioritize time to schedule patients in the primary care clinical pharmacy clinic that I established collaboratively with our USF Health Morsani College of Medicine – Department of Family Medicine almost 20 years ago. Years ago, during that same patient encounter, I asked my patient, who was 84, if she would be able to schedule a return visit on a particular date in the near future. She said “Let me see,” and proceeded to pull out an Ipod. I sat there mildly amazed at how nimble she was with the device, and how accepting she was of the information that she retrieved from her device. I asked her how she felt about the device, and if she would be open to utilizing the device for health-related education and activities. She expressed that she would not only be open to the idea, but added how she felt that such technologies could provide her with more timely information “on her time,” and not someone else’s. It strengthened my belief that emerging mobile health technologies are an essential component for optimizing patient engagement.
Effective medication therapy is at the core of managing patients with chronic disease states, such as diabetes or hypertension. Unfortunately, medication therapy in this country has been far less than optimal, and in some cases creates harm (1). Through multiple studies and reviews, it is well known that 50% of medications prescribed by health providers are not taken as prescribed within six-months, and 25% of prescribed medications are never filled or picked up (2). Prescribers, most notably physicians, simply do not have the additional time or focus to follow behind patients about these medication challenges. Pharmacist clinicians offer the best opportunity to not only improve adherence, but to measure and monitor the effectiveness and potential barriers to successful medication optimization (3). Using mobile health technologies, these monitoring and measurement technologies create improved connectivity with patients in their daily ambulatory lives without requiring additional timely and costly visits to healthcare clinics.
I also foresee the possibility of bringing these technologies into underserved and underrepresented communities, which are often affected the most by lack of healthcare access. Putting these technologies into the hands of community health workers and other “health extenders”, with proper medical provider supports, could become an effective means of improving health disparities in many communities. Decreased emergency room visits and hospital readmission rates can be achieved, while creating an inclusive environment where people from all communities can benefit from emerging health technologies. Ultimately, poor health in any community is a drag on all communities. The public health impact holds so much promise with the implementation of these technologies.
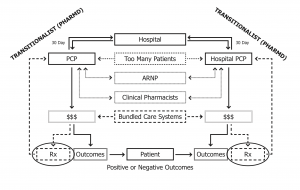
In my two most recent posts (Time for Pharmacists to Move from Behind the Counter and Interprofessional Health Initiatives- Health Systems Cannot Succeed Without Them!) I expressed that Interprofessional Clinical Collaborations simply must evolve to achieve optimal health outcomes. Interoperability of electronic platforms, Collaborative Practice Agreements, and capitated reimbursement models for clinical services will provide pathways for pharmacist clinicians to optimize medication outcomes as members of patient-centered healthcare teams. Status quo healthcare delivery, siloed health providers, and avoidance of emerging health technologies will certainly stifle opportunities for our national and regional healthcare systems to provide the most outstanding healthcare at lower costs. Mobile health technologies offer the best opportunity to initiate new communication paradigms between patients and their health provider teams. The Time is Now to embrace mobile health technologies.
- Watanabe JH, McInnis T, Hirsch JD. Cost of prescription drug-related morbidity and mortality. Ann Pharmacotherapy. 2018;52(9):829-837.
- Viswanathan M. Golin CE, Jones CD, et al. Intervention to improve adherence to self-administered medications for chronic diseases in the United States: as systematic review. Ann Intern Med. 2012;157(11):785-795
- https://www.pharmacist.com/article/acos-can-do-more-medication-optimization-study-says (accessed 06/04/2019)