University of South Florida neonatologist Akhil Maheshwari, MD, and his team advance research to understand, detect and identify novel treatments for necrotizing enterocolitis, or NEC, a life-threatening inflammatory bowel disease that may afflict premature newborns.
“As we’ve become better at controlling lung disease in premature infants, NEC has emerged as the single largest killer of premature babies,” said Dr. Maheshwari, a physician-scientist who holds the Pamela and Leslie Muma Endowed Chair in Neonatology in the Department of Pediatrics, USF Health Morsani College of Medicine. Dr. Maheshwari also serves as medical director of the Jennifer Leigh Muma Neonatal Intensive Care Unit (NICU) at Tampa General Hospital.

Akhil Maheshwari, MD, holds the Pamela and Leslie Muma Endowed Chair in Neonatology in the USF Health Department of Pediatrics.
![]() Listen to Dr. Maheshwari talk about the impact of NEC.
Listen to Dr. Maheshwari talk about the impact of NEC.
The serious gastrointestinal disorder happens when the small or large intestine becomes inflamed and the lining of the intestinal wall starts to die off. In the United States, it affects up to 10 percent of extremely low birth weight infants (less than 3.5 lbs.), with a mortality rate of 50 percent. Among premature infants in developing countries, such as India or China, NEC is more common.
With advances in technology and best clinical care practices, more extremely preterm infants are surviving with fewer complications, but NEC remains one of the most challenging diseases confronting neonatologists and pediatric surgeons. The causes of the dreaded condition remain unclear, and there is no treatment.
Translational research enlightened by clinical experience
Caring for tiny, fragile patients in Tampa General Hospital’s NICU adds perspective to the research Dr. Maheshwari conducts in his laboratory at the Morsani College of Medicine. “The vantage point I have as a neonatologist lets me observe NEC in the clinical setting, and I strive in the laboratory to translate this information to understand its pathophysiology,” said the USF Health professor of pediatrics, molecular medicine, and public health.
Over the last decade, Dr. Maheshwari’s group, and others, have found that a third of all instances of NEC in extremely premature infants occurs within 48 hours of receiving a blood transfusion. He was recently awarded a five-year, $1.5-million R01 grant from the National Heart, Blood and Lung Institute, National Institutes of Health, to understand how blood transfusions may cause bowel injury in premature infants and develop new ways to prevent or treat this condition.

The newborn patients treated at Tampa General Hospital’s Muma Neontal Intensive Care Unit by Dr. Maheshwari, the unit’s medical director, are the among the most fragile and sickest.

In the U.S., necrotizing enterocolitis, or NEC, affects up to 10 percent of extremely low birth weight infants (less than 3.5 lbs.), with a mortality rate of 50 percent. Causes of the life-threatening inflammatory bowel disease, a focus of Dr. Maheshwari’s research, remain unclear.
![]() Dr. Maheshwari discusses his latest NIH grant.
Dr. Maheshwari discusses his latest NIH grant.
Supported by the latest NIH grant, Dr. Maheshwari will use a newborn mouse model to test whether red blood cell transfusions induce intestinal injury, whether the underlying anemia present in almost all premature newborns aggravates this injury, or whether both play a role in causing NEC. The USF researchers will also evaluate whether several standard blood bank practices — longer red blood cell storage, red blood cell washing to remove potentially hazardous electrolytes, and irradiation of transfused blood to help reduce risk of infection — can alter the severity of intestinal injury.
While many critically ill premature infants are stabilized within their first two weeks in the neonatal intensive care unit, within the second to third week a small proportion experience rapid onset of NEC without warning. “I see infants in the unit who were doing well and then die suddenly,” Dr. Maheshwari said. “The impact of this disease can be devastating, both emotionally and in terms of health care costs.”
There is no definitive diagnostic test to identify the disease in its earliest stages; abdominal X-rays can only diagnose when NEC has progressed to severe intestinal damage, including sometimes bowel perforation or peritonitis, Dr. Maheshwari said. Consequently, clinicians err on the side of caution if they suspect NEC — monitoring the condition with X-rays and extensive bloodwork, halting regular feedings, administering IV fluids and antibiotics and counseling an anxious family about what to expect if a NEC diagnosis is confirmed.
“The number of infants in the NICU who undergo testing for NEC is about 10 times more than the number who actually have the disease,” he said.
Half of the babies with confirmed NEC require surgery to excise the damaged intestinal tissue, and 50 percent who go to the operating room die, Dr. Maheshwari said. “The other half who survive end up with anatomically short intestines, so they depend on IV nutrition and often develop nutritional and developmental deficiencies that can affect brain growth. They are at risk for lifelong complications.”
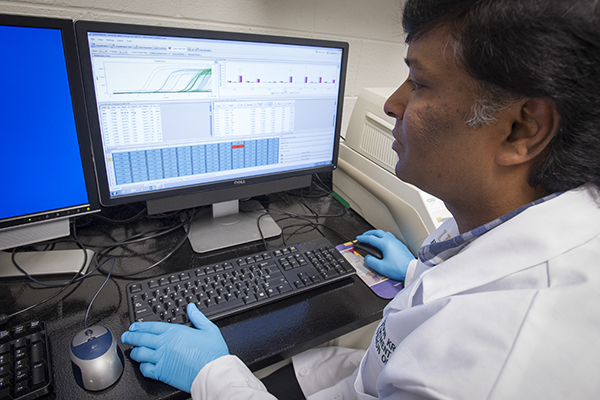
Mohan Kumar Krishnan, PhD, a research associate in Dr. Maheshwari’s laboratory, uses quantitative real-time polymerase chain reaction (PCR) to monitor amplification of gene expression. The technique helps the researchers determine how the immune system is responding to bacteria in the gut.
Key findings of Dr. Maheshwari’s laboratory
Researchers now believe that three things must all be present in the premature infant’s gut for NEC to occur: bacteria, inflammation, and a unique signature of white blood cells (monocytes and macrophages) not found in adults with inflammatory bowel diseases.
In addition to the study of red blood cell transfusion-associated NEC, Dr. Maheshwari’s team focuses on two other lines of investigation — determining whether modifying the premature infant’s feedings can alter the immature, hyper-inflammatory nature of macrophages and identifying how the bowel’s inflammatory response in a premature infant differs from that in an adult, so the macrophages might be modified to prevent or treat NEC. The researchers hypothesize that the aggravated inflammatory response seen in the bowels of preterm infants happens because these very small babies with immature immune systems have not yet formed the adaptive mechanisms needed to tolerate the bacteria in their guts.

Dr. Maheshwari (center) with his research team, from left to right: Mohan Kumar Krishnan, PhD, research associate; Tanjing Song, PhD; senior biological scientist; Chitra Palanivel, PhD, postdoctoral research scholar; Kopperuncholan Namachivayam, PhD, research associate; and Thais Queliz Pena, MD, neonatology fellow.
Among some of their most significant findings:
- First to show that premature infants may be at risk of NEC because of a lack of the protein known as transforming growth factor-β2 (TGF-β2), which suppresses inflammatory responses.
- Demonstrated that infants whose bowel injury escalates to NEC have low blood levels of TGFβ2 since birth. “TGFβ2 is the first biomarker that can be obtained on day 1 to help predict which infants are most likely to develop NEC. Its 60-percent accuracy rate is still a six-fold improvement over the way we predict NEC now – by degree of prematurity,” Dr. Maheshwari said.
- While mothers who deliver preterm infants produce breast milk containing a large amount of TGF-β2, Dr.Maheshwari found that the beneficial growth factor in the mothers’ milk is largely biologically inactive. The USF researchers are investigating ways to activate the mother’s milk-borne TGFβ2 – in essence stimulating the milk to undergo the maturation needed to suppress unnecessary inflammation and protect the baby against NEC.
- Discovered that an acute drop in monocyte count in premature infants could be used as a diagnostic test to differentiate NEC from more benign causes of feeding intolerance like prematurity itself. A study led by Dr. Maheshwari found that 70 percent of premature infants with NEC experienced more than a 20-percent drop in monocytes in their blood.
- Recently identified a unique subtype of monocyte, formed in the newborn’s liver, which infiltrates the intestine of premature infants and may promote bowel injury. The subtype could be a new target for treating NEC.
![]() Dr. Maheshwari gives an example of how a laboratory discovery may change clinical practice.
Dr. Maheshwari gives an example of how a laboratory discovery may change clinical practice.

Dr. Maheshwari was recently awarded a five-year, $1.5-million R01 grant from the NIH’s National Heart, Blood and Lung Institute to study how blood transfusions may cause bowel injury in premature infants and develop new ways to prevent or treat this condition.
In addition to his NIH-supported NEC research, Dr. Maheshwari has a $143,000 American Heart Association grant to study ways to block systemic inflammation and multi-organ dysfunction in very ill babies put on a treatment known extracorpeal membrane oxygenation (ECMO), which uses a heart-lung bypass machine.
“Dr Maheshwari’s work is highly innovative and has relevance well beyond the field of neonatology,” said Patricia Emmanuel, professor and chair of pediatrics at the USF Health Morsani College of Medicine. “He brings great curiosity and passion to his research and is a wonderful role model for fellows and residents.”
Endowment key to research benefitting tiniest newborns
The endowment by Pam and Les Muma to advance USF-TGH research and care for the sickest newborns helps support the infrastructure of Dr. Maheshwari’s highly specialized laboratory, including a machine that can measure a drop of a blood so tiny it fits on the head of a pin.
“Endowments are so critical,” Dr. Maheshwari said. “The equipment needed for the type of research we do is very specific for premature newborns, and doesn’t exist in most universities.”
Dr. Maheshwiari came to USF in 2014 from the University of Illinois at Chicago (UIC), where he was an associate professor pediatrics and chief of the Division of Neonatology. Prior to his tenure at UIC, he was an assistant professor at the University of Alabama at Birmingham and received several young investigator awards, including the American Gastroenterological Association Research Scholar Award and the Procter and Gamble GI Scholar Award.

The Muma endowment supports highly specialized equipment in Dr. Maheshwari’s neonatal research laboratory, including a machine that can measure a drop of a blood so tiny it fits on the head of a pin.
Dr. Maheshwari is a member of the editorial board of Maternal Health, Neonatology and Perinatology and several other professional journals and served on several grant review panels. He holds six provisional patents for new anti-inflammatory agents.
He earned his medical degree from the Institute of Medical Sciences, Varanasi, India, completed a pediatrics residency at the University of Florida, and received fellowship training in neonatology at USF.

Dr. Maheshwari with research associate Kopperuncholan Namachivayam, who works at a hematology analyzer that counts and separates various blood cell types including immune cells the researchers are interested in studying.
Photos by Eric Younghans, USF Health Communications
