Seeking to understand how the heart short circuits, Sami Noujaim looks for new drugs to fix atrial fibrillation
Within the last three years, USF biomedical scientist Sami Noujaim, PhD, lost his older brother to sudden cardiac death and his 80-year-old father was diagnosed with atrial fibrillation.
The experiences gave Dr. Noujaim a new appreciation for his research on understanding how normal and abnormal electrical impulses are generated in the heart. The Cardiac Electrophysiology Research Laboratory he directs focuses on finding more effective drugs to treat atrial fibrillation, the most common irregular heart rhythm and a condition for which prevalence rises markedly after age 65.
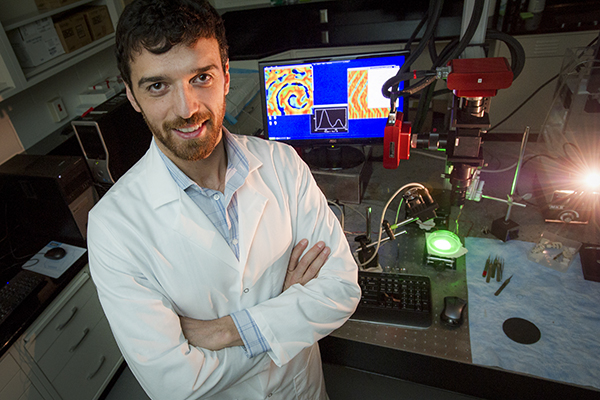
Sami Noujaim, PhD, directs the Cardiac Electrophysiology Research Laboratory in the USF Health Department of Molecular Pharmacology and Physiology.
“When life throws something like that at you, the work you do takes on a more personal tone, a sense of mission. I realized that neither myself nor my loved ones are immune from the cardiovascular diseases I’m studying,” said Dr. Noujaim, an assistant professor in the Morsani College of Medicine’s Department of Molecular Pharmacology and Physiology. “We are all at risk.”
![]() Dr. Sami Noujaim describes the focus of his laboratory’s research.
Dr. Sami Noujaim describes the focus of his laboratory’s research.
Searching for noninvasive solutions to atrial fibrillation
Atrial fibrillation is a problem with the cardiac electrical circuitry that controls the rate and rhythm of the heartbeat. The condition affects about 9 percent of the U.S. population age 65 or older, according to the Centers for Disease Control and Prevention, and can lead to potentially deadly complications such as stroke and heart failure. While signs of atrial fibrillation may include heart palpitations, fatigue, lightheadedness, dizziness and shortness of breath, some people experience no noticeable symptoms.
Treatment and management options include lifestyle changes, medications to help control heart rate and rhythm and reduce the risk of blood clots, controlled electrical shock (cardioversion to reset heart rhythm), invasive procedures (catheter ablation) and surgical implantation of pacemakers. However, a major challenge is that atrial fibrillation frequently recurs after normal heart rhythm (sinus rhythm) is restored.
“The existing treatments can be good, but there is a lot of room for improvement, so we are focusing on contributing to noninvasive treatment options,” Dr. Noujaim said. “If we could help physicians get patients with atrial fibrillation to long-term normal sinus rhythm, and perhaps increase the ability to take them off blood thinners, it would be a significant improvement.”
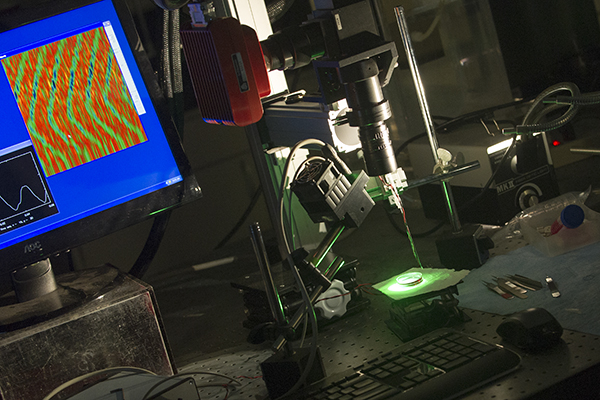
Dr. Noujaim’s laboratory uses specialized equipment to measure the electrical activity of heart muscle cells and image what he describes as “atrial fibrillation in a dish.”
Closing in on a pathway linking aging and Afib
Dr. Noujaim currently works with colleagues at USF and other institutions, including Tufts University, the University of Michigan, and Northeastern University, to investigate how age-related changes in specific potassium ion channels known as GIRK may trigger a cascade of molecular events leading to atrial fibrillation. His research, supported by a five-year $2.14 million RO1 grant from the National Heart, Lung and Blood Institute employs techniques including structural biology, molecular simulations, and cellular and whole organ electrophysiology.
The researchers hypothesize that in aging-associated atrial fibrillation, the condition may arise when a biochemical pathway controlling the GIRK postassium channels begins behaving abnormally, in part because of structural and metabolic cardiovascular changes that occur with aging. High blood pressure, diabetes, and coronary artery disease– among the most common risk factors for atrial fibrillation – become more common as people grow older.
At USF, Dr. Noujaim collaborates with Javier Cuevas, PhD, in Molecular Pharmacology and Physiology, Michael Teng, PhD, in Molecular Medicine and in Allergy and Immunology, and Juan Del Valle, PhD, in Chemistry to investigate ways to target and block the GIRK potassium channels using pharmacological approaches that rely on immunology and chemistry.

Mohammed Alhadidy (left), a biomedical graduate student, and Bojjibabu Chidipi, PhD, a postdoctoral scholar in Molecular Pharmacology and Physiology, record the electrical signals from several cells using a multichannel automated patch clamp.
![]() The significance of investigating the relationship between aging and atrial fibrillation.
The significance of investigating the relationship between aging and atrial fibrillation.
Designing a “perfect plug” using an antimalarial drug model
“Right now, we are trying to design a perfect plug using the antimalarial drug chloroquine as a model,” Dr. Noujaim said, “We have evidence that if we block that specific type of potassium channels we will be able to stop atrial fibrillation or at least reduce its occurrence.”
Earlier work by Dr. Noujaim and others, including a study reported in the journal FASEB, demonstrated that the antimalarial drug chloroquine was effective in blocking the GIRK potassium channels and suggested a new path for discovering antiarrhythmic drugs.
Dr. Noujaim continues using cellular and animal models to pinpoint how and where the chloroquine molecule interacts with the potassium channel – with the aim of discovering a “plug” that works even better than the antimalarial drug. At the same time, he has reached out to USF Health Department of Cardiovascular Sciences to begin applying the laboratory findings to the clinic.
Working with cardiologists Bengt Herweg, MD, and Dany Sayad, MD, Dr. Noujaim recently gained approval for a pilot study to enroll 40 adults without heart damage whose atrial fibrillation has persisted more than one week and less one year. The team will test the effectiveness of chloroquine in restoring and maintaining normal heart rhythm in patients with atrial fibrillation.
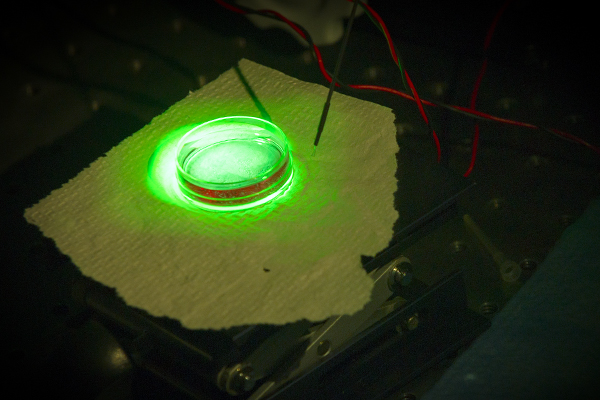
The laboratory uses techniques including structural biology, molecular simulations, and cellular and whole organ electrophysiology to conduct its NIH-funded research.
Collaborating with clinicians on new treatment options
Dr. Sayad, initially surprised at Dr. Noujaim’s proposal to try chloroquine, said the strength of the preclinical data convinced him of the antimalarial drug’s potential as another antiarrhythmic option. “Treating atrial fibrillation can be especially challenging in older patients, who experience a higher recurrence of atrial fibrillation (following cardioversion) and more failure on drugs used to regulate heart rhythm,” he said.
Clinicians help biomedical scientists like Dr. Noujaim frame and focus their studies to make the research more relevant to challenges faced in treating patients, such as maintaining sinus rhythm once a normal heartbeat has been restored.
“It does not mean that the fundamental, basic science questions are not important,” Dr. Noujaim said. “To the contrary, those questions are at the heart of every single experiment we do; however, we must always think about the big picture and why we are asking those questions. And that always goes back to the clinic.”
In previous electrophysiology experiments, Dr. Noujaim and colleagues helped better define the contribution of the nervous system within the heart, otherwise known as the intrinsic cardiac ganglia, to normal and abnormal heart rhythm. Using both mouse models and patients with atrial fibrillation, the study shed light on how nerves emerging from these cardiac ganglia regulate activity of the sinus node, the heart’s natural pacemaker. The study appeared in Cardiovascular Research in 2013.

Dr. Noujaim with members of his research team, from left, Bojjibabu Chidipi, Mohammed Alhadidy and laboratory manager Michelle Reiser.
![]() Dr. Noujaim comments on the importance of a clinical perspective to frame biomedical research.
Dr. Noujaim comments on the importance of a clinical perspective to frame biomedical research.
Impressed by USF’s biomedical research opportunities
Dr. Noujaim came to USF in 2015 from the Molecular Cardiology Research Institute at Tufts University School of Medicine. He received his PhD in pharmacology, with distinction, from SUNY Upstate Medical University in Syracuse, NY, followed by a year of postdoctoral training there. He then completed a three-year postdoctoral fellowship, supported by the American Heart Association, and the National Institutes of Health, at the Center for Arrhythmia Research, University of Michigan, in Ann Arbor, MI.
Dr. Noujaim said he was attracted to USF by the opportunity to be part of an emerging preeminent university committed to establishing a cardiovascular institute bridging top biomedical research and clinical care.
“The opportunities that the University of South Florida is providing for scientists are equal or greater than those at any other major academic medical center,” he said. “It was also striking to me that, in a place the size of USF, the USF Health leadership is so actively engaged in research, with their own laboratories and grants. That’s not what you would see in a lot of places, and as a biomedical scientist it makes me feel that the leadership here really values research.”

Dr. Noujaim is passionate about the cardiovascular research his laboratory conducts, which he says has taken on a greater sense of mission since his own family’s experience with sudden cardiac death and atrial fibrillation.
![]() His take on the benefit of brainstorming with scientists in other disciplines.
His take on the benefit of brainstorming with scientists in other disciplines.
Some things you may not know about Dr. Noujaim:
- Born in Lebanon, he moved to the United States after graduating from high school.
- He routinely swims laps in an indoor pool.
- He enjoys experimenting with cooking, specializing in inventing new dishes by combining ingredients he finds in his refrigerator. “I’ve discovered by trial and error that no matter how bad what I cook really is, adding a tablespoon of soy sauce makes it alright,” he said.
- His first scientific experiment as a college student volunteering in Boston’s Beth Israel Deaconess Medical Center laboratory was unforgettable. He fainted while his blood was being drawn so he could use it to help study blood platelet activation and aggregation. Click on video below to find out more.
-Photos and video by Eric Younghans, and audioclips by Sandra C. Roa, USF Communications and Marketing
