Drawing on the expertise of regional physicians, including experts from USF Health, U.S. Rep. Ross Spano recently hosted a discussion about the impact telehealth could have during the current COVID-19 pandemic.
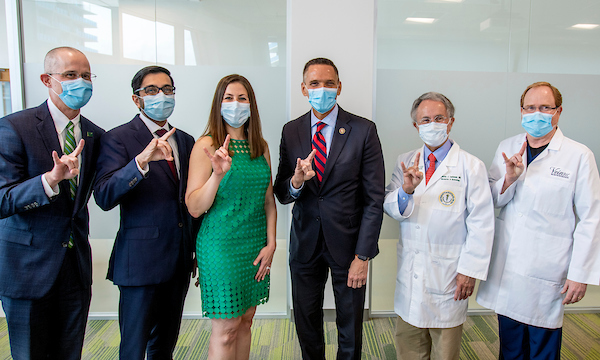
U.S. Rep. Ross Spano (FL-15) hosted a roundtable discussion at USF Health’s Morsani College of Medicine downtown Tampa June 2, with medical professionals, including USF Health doctors, on how COVID-19 has changed telehealth. From left, Dr. Mark Moseley, Dr. Nishit Patel, Dr. Eva Crooke, Rep. Ross Spano, Dr. Charles Lockwood and Dr. Chris Pittman.
Called How Telemedicine Can Help w/COVID-19, the roundtable conversation was held June 2 in the newly opened USF Health Morsani College of Medicine and Heart Institute in downtown Tampa.
The event offered an exchange of ideas for how telehealth is impacting patient care during the current COVID-19 pandemic and while patients follow stay-at-home guidelines, and telehealth’s place in future health care offerings once COVID-19 dies down or there is a vaccine.
The physicians represented a range of specialties, offering a better sense for the areas of health care that could make the best use out of telehealth.
Roundtable participants included:
- Eva Crooke, MD, the Women’s Group. Her specialty is obstetrics and gynecology.
- Charles J. Lockwood, MD, MHCM, senior vice president for USF Health and dean of the Morsani College of Medicine. His specialties are obstetrics and gynecology and maternal-fetal medicine.
- Mark G. Moseley, MD, MHA, CPE, chief clinical officer for USF Health. His specialty is emergency medicine.
- Nishit Patel, MD, FAAD, associate professor and chief medical information officer. His specialty is dermatology.
- Chris Pittman, MD, Vein 911. His specialties are radiology, and venous and lymphatic medicine.
- S. Rep. Ross Spano, Representative of the 15th District since 2019.
What they said…

Dr. Charles Lockwood: “We’ve learned a lot about its limitations and a lot about its potential… It needs to stay because I think it has a place.” On the downside of telehealth: “There’s always the risk of missing something. We depend so much on clues that are often very hard to define. Might be the expression on a patient’s face, it might be a physical exam finding. So you miss that, literally, that physical contact…It’s up to the physician to understand the limits of the technology.”
Dr. Mark Moseley: “One of the things I think is a concern is that it doesn’t apply equally to all specialties. For a practice like psychiatry it works really well. In fact, I think they’re seeing more patients now through telehealth than what they did before. Some specialties like dermatology or ophthalmology, where it’s a highly specialized field or there are parts of the physical exam that require special equipment, just aren’t quite as good. So, it gets to the issue of use cases and if you pick a good use case for the technology the technology enables you to do that. If you pick a poor use case, then that clearly is a risk. Because you might assume you’re able to do everything but you can’t… We’ve learned a lot during that period of time (since telehealth) and some of it is learning what we can and can’t do. And realizing you’re going to have to pick the right use for it. It’s a tool for us, no different than a stethoscope or something we have in our specialties. But if we use the tool incorrectly, that’s when the risk comes in.”
Dr. Nishit Patel: “For dermatologists, one of the things that we do a lot of is skin cancer monitoring for melanomas and for other things. That’s one of the things that, in order to do a really good job, you have to get high-quality photos, and use a special magnifying lens to look at it… Some guidelines exist but with the whole country moving so quickly to telehealth, we’re going to get a lot of good literature out of this to try and expand on what are the appropriate diagnoses and appropriate cases (for telehealth). And the other thing that really important to mitigate some of that potential risk is being able to have the fluid situation between seeing a patient in telehealth and if you need to see them in person. If you already have that existing relationship, you can say why don’t we have you come in …Having that existing relationship for not only telehealth visits but also with a continuum to in-person care.”
Dr. Eva Crooke: “It will definitely not replace what we do in the office. It’s a good adjunct where we can utilize it in addition. It definitely makes for a lot better efficiency. We noticed that as probably the biggest piece in our practice where we can see more patients, they’re satisfaction rates on wait times, without any other piece of their satisfaction scores, is a huge difference. So I think it will be used as a tool intertwined into the way we practice right now, assuming we can keep the barriers minimal.”

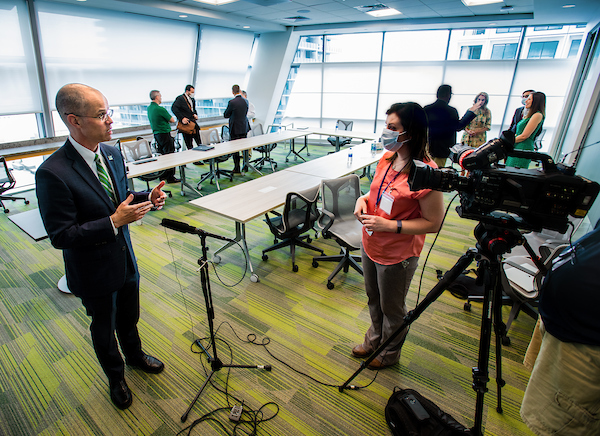
Dr. Charles Lockwood provided Rep. Ross Spano with a tour of the new building, which opened in January 2020.
Photos by Allison Long, USF Health Communications.
