A USF Health study applies a new mouse model of tauopathy, which may help identify therapeutic targets for Alzheimer’s and other neurodegenerative diseases
TAMPA, Fla (April 20, 2021) — Chaperone protein imbalance can play a significant role in initiating toxic accumulation of tau in the aging brain – an early step in the development of Alzheimer’s disease and related neurodegenerative disorders known as tauopathies, a new preclinical study by University of South Florida Health (USF Health) neuroscientists suggests.

Laura Blair, PhD, assistant professor of molecular medicine at the USF Health Byrd Alzheimer’s Center, was principal investigator for the NIH-funded study published in Acta Neuropathologica Communications | Photo by Allison Long, USF Health Communications
In humans, misfolding of the protein tau leads to its toxic accumulation inside brain cells, the formation of these tau aggregates into hallmark neurofibrillary tangles, neuron death, and eventually symptoms of cognitive decline such as memory loss and diminished thinking skills.
In this study the USF Health Morsani College of Medicine researchers used mice that were not genetically modified (wild-type mice) to examine the effects of Aha1 and FKBP52, two co-chaperone proteins of heat shock protein Hsp90, in the aging brain. They modeled molecular chaperone imbalance by overexpressing production of Aha1 and FKBP52 in these old, wide-type mice. The findings, highlighted below, were reported April 8 in Acta Neuropathologica Communications.
Hsp90 is a chaperone protein abundant in neurons and other cells in the brain. Normally, co-chaperone proteins assist chaperone proteins in monitoring and sustaining the balance (homeostasis) of proteins critical to cell health.
“The chaperone protein network is your cell’s natural defense to maintain homeostasis throughout life, and this study emphasizes the importance of protecting that balance in the aging brain,” said principal investigator Laura Blair, PhD, an assistant professor of molecular medicine at the USF Health Byrd Alzheimer’s Center, Morsani College of Medicine. “We’re excited about using this new model of tauopathy in finding ways to restore chaperone protein balance to delay or stop the progression of Alzheimer’s and other neurodegenerative diseases.”

Dr. Blair along with the research paper’s co-lead authors Marangelie Criado-Marrero, PhD (left), a postdoctoral fellow, and Niat Gebru (center), a doctoral student. | Photo by Allison Long
Among their many quality-control functions, chaperone protein networks ensure proteins are folded to conform to the proper 3D shapes, transported precisely where needed to do their jobs, and pushed toward degradation if they are abnormally modified or no longer useful. Heat shock proteins like Hsp90, triggered when a cell is under stress, play a particularly important “triage” role in correcting protein misfolding to prevent aggregation.
“But in the aging brain, the balance of the chaperone proteins shifts and creates a system not working as efficiently as it normally would. Large numbers of the chaperone molecules decrease in expression, and a smaller but significant number increase in their expression,” Dr. Blair said.
Increasing age is the greatest known risk factor for Alzheimer’s disease. So, the USF Health team investigated whether increased levels of FKBP52 and Aha1 alone could initiate pathological features mimicking human Alzheimer’s disease in aged wild-type mice – those with no genetic manipulations predisposing their brains to abnormally increase tau aggregation.
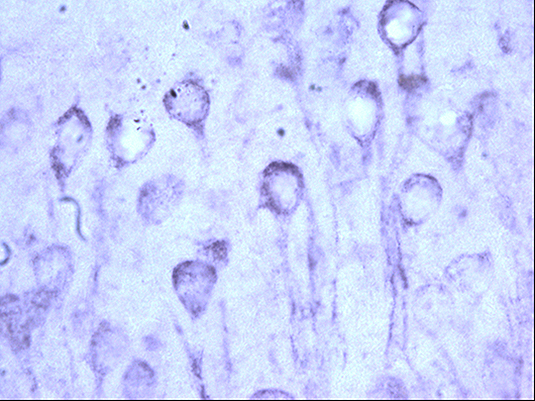
Tau pathology resembling that seen in Alzheimer’s disease brains. | Image courtesy of Laura Blair laboratory, USF Health
Key findings from their new mouse model of tauopathy include:
- High levels of FKBP52, and to a lesser extent elevated levels of Aha1, increased tau accumulation over time in the aged, wild-type mice.
- The tau accumulation promoted by overexpression of FKBP52, but not Aha1, correlated with increased neuroinflammation through exaggerated activation of neuronal support cells, namely microglia and astrocytes. This was complemented by loss of neurons and cognitive impairments.
Existing mouse models, including those that add or subtract genes, introduce tau mutations, and seed mice brains with human tau, help scientists learn more about the underlying causes of Alzheimer’s disease and other tauopathies. However, they tend to be limited in capturing the physiological aspects of neurodegeneration in the context of both normal and abnormal aging.
“We hope this (chaperone imbalance) model will help us better understand the dynamics of tau aggregation and neuroinflammation, including the timing and connections among pathological events, without directly regulating one pathway or the other,” Dr. Blair said.
Dr. Blair’s team has designed follow-up studies to help unravel if, and when, tau accumulation or neuroinflammation is more influential in causing brain cell toxicity during aging. That could help determine which chaperones — FKBP52, Aha1, or others — may be the best therapeutic target options for restoring protein balance, she said.

Dr. Blair’s laboratory studies how various chaperone proteins interact, for better or worse, with different forms of tau – ranging from soluble tau protein that can spread from one brain cell to another to the aggregated, misfolded neurofibrillary tangles inside brain cells.
Co-lead authors for the USF Health study were postdoctoral fellow Marangelie Criado-Marrero, PhD, and doctoral student Niat Gebru. The research was supported by grants from the National Institutes of Health/National Institute of Neurological Disorders and Stroke and the National Institute of Mental Health.
