The USF Health College of Public Health (COPH) Doctor of Public Health (DrPH) program emphasizes advanced public health education and training designed to prepare individuals for leadership roles in practice-based settings. Traditionally, the program is taught through a hybrid format of primarily distance-learning courses and three, five day on-campus institutes, but COVID-19 forced these live in-person institutes to shift to virtual delivery in 2020 through Microsoft Teams. The program is designed for working professionals in the public health field, with most recent cohorts averaging five or more years of field experience, to gain the opportunity to connect and collaborate with other doctoral students in both the DrPH and PhD programs and strengthen their skills for public health leadership, practice and research without interrupting their careers. These doctoral students come from a wide range of fields including epidemiology, county and state level disaster and emergency preparedness and response, health education, health law, laboratory operations management, maternal and child health, social work, food insecurity, and others. They work across federal and state government agencies along with local county health departments, healthcare organizations, non-profits, universities, consulting practices, to name a few.
COVID-19 clearly had other plans in mind for the program and for the careers of current USF Health DrPH students who immediately became key parts of COVID-19 operations across the country and abroad. These students stepped up, represented public health in their organization’s interprofessional teams and really demonstrated the College of Public Health’s motto, “our practice is our passion.” The following biographical sketches provide summaries of the backgrounds and a focus on the roles these DrPH students are contributing in their communities in the fight against COVID-19.
 Stephanie Anspaugh-Naples, MPH
Stephanie Anspaugh-Naples, MPH
State Medical Countermeasure (MCM) Coordinator, Florida Department of Health (DOH)
PINELLAS COUNTY, FL – Anspaugh-Naples’ job on a daily basis is to help plan for the mass dispensing and mass vaccination of the State of Florida. The importance of her role heightened when COVID-19 broke out and once the vaccines became available, “all the work we’ve done to build partnerships, upgrade systems and learn from previous responses will be put to the test,” Anspaugh-Naples said. “It’s exciting and terrifying.”
In addition to being the chairperson for the Association of State and Territorial Health Officials (ASTHO) MCM Coordinators Workgroup, she is currently part of the state’s COVID-19 Response Team for Emergency Support Function 8 – Public Health and Medical (ESF-8) and leads the COVID-19 Mass Vaccination Planning Workgroup. “We are developing strategies to ensure that everyone in the state will have access to a COVID-19 vaccine as doses become available,” Anspaugh-Naples said. “Florida is a very diverse state, so we are engaging other agencies and organizations to work through existing channels to expand our ability to reach everyone in the state.”
Anspaugh-Naples is based out of Pinellas County, Florida, but the rest of her Bureau working on this effort together is in Tallahassee. Her work in public health response is always a collaborative effort and when it’s all-hands-on-deck for an outbreak like COVID-19, the teamwork not only includes internal partners at DOH but also other state agencies, community partners, the Florida Division of Emergency Management, Florida Hospital Association, American Medical Response, International Medical Corps, county emergency management agencies and many others. “Relationships are a critical part of preparedness and response work,” Anspaugh-Naples said.
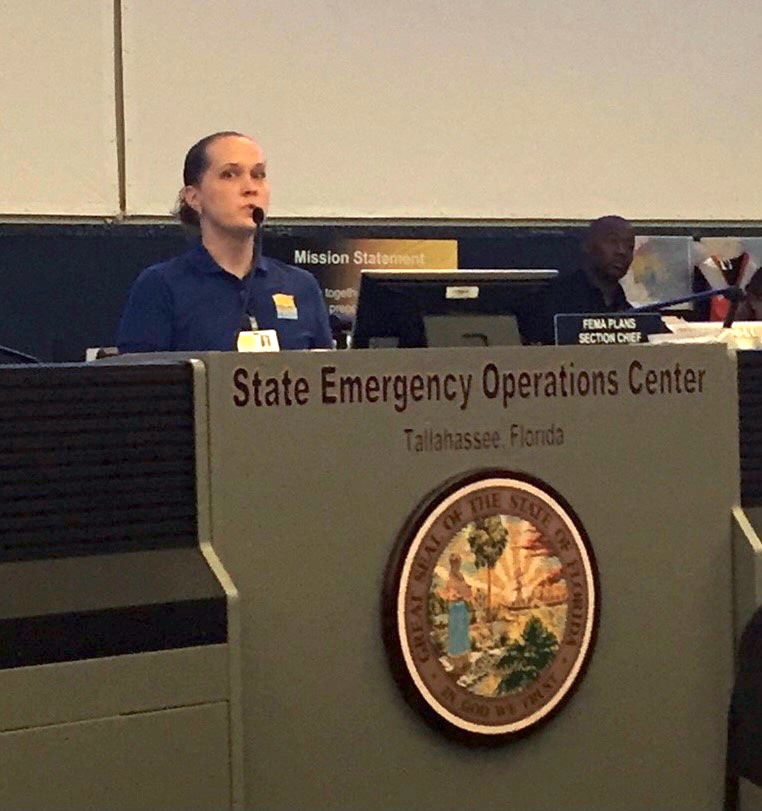
Stephanie Anspaugh-Naples at the State Emergency Operations Center in Tallahassee, Florida. (Pre-COVID photo courtesy of Anspaugh-Naples)
Originally a USF Bull, Anspaugh-Naples’ educational background includes a Bachelor of Science in Biology from USF and a Master of Public Health in Epidemiology from Emory University. In 2016, she returned to her alma mater for the DrPH program because it was the only program that was flexible enough for a working professional and had the ability to tailor the education based on her interests. “When I looked at other public health doctoral programs, there wasn’t another DrPH program that paralleled USF’s,” Anspaugh-Naples said. “I only applied to USF and my plan was to continue applying until I got in. Thankfully, I was accepted on my first try but I was ready to be persistent for however long it took.”
Her studies in the program have focused on public health preparedness and response and systems thinking/theories. Since Anspaugh-Naples started the program prior to COVID, she was able to participate in an in-person fall institute. In her first class, Joe Bohn, PhD, MBA, assistant professor and deputy director of the USF Health DrPH Program, covered systems thinking and similar theories which really resonated with her. Dr. Bohn soon became her faculty advisor and has helped her shape her doctoral project. Through discussions with Dr. Bohn and Marissa Levine, MD, MPH, FAAFP, professor and director of the USF Health Center for Leadership in Public Health Practice (CLPHP), about her doctoral project, she learned about Cynefin, a conceptual framework used to aid decision-making. “When the COVID-19 Mass Vaccination Planning Workgroup first started, I shared a graphic of the Cynefin framework with the team,” Anspaugh-Naples said. “Planning a mass vaccination campaign with so many unknowns has been a challenge but employing concepts from Cynefin helped me to focus on what we do know, rather than on what we didn’t/don’t know.”
COVID-19 has reinforced her passion for public health preparedness and response. “There’s a certain ebb and flow to the work that ensures I’m never bored or unchallenged and I appreciate that. Plus, I feel like the work I’m doing helps people, even if they never know I’m doing it,” Anspaugh-Naples said.
Planning a state mass vaccination campaign has slowed down the progress Anspaugh-Naples wanted to make on her doctoral plan, but she’s grateful to have friends in her cohort who are in a similar position and remind her that, “every step, no matter how small, is still a step forward.” Anspaugh-Naples stresses the importance of maintaining professional working relationships and she feels that the best part of the DrPH program has been her ability to build those lasting relationships with her classmates and professors.
 Jarad Schiffer, MS
Jarad Schiffer, MS
Supervisory Health Scientist and Advisor for Laboratory Preparedness, Centers for Disease Control and Prevention
ATLANTA, GA – At the beginning of the outbreak, Schiffer was running an immunology laboratory at the Centers for Disease Control and Prevention (CDC). In March, his team was asked to stand up serology testing for COVID surveillance. “We took a research assay to measure anti-Spike IgG and modified it to increase the throughput from 10 specimens/run to 88 specimens/run, validated it using ~100 PCR-confirmed COVID samples and ~300 negative samples we had left from pre-COVID studies,” said Schiffer. “From April to October we tested a little over 112,000 specimens. Our data was the basis for Dr. Redfield’s interview where he indicated that there were ~10 unconfirmed cases for each confirmed case.”
Schiffer’s laboratory was originally set up for the Anthrax Vaccine Research Program and then they went on to work on the Pertussis vaccine as well as provide laboratory support for the 2009 H1N1 outbreak, the 2014 Ebola outbreak and STRIVE vaccine trial, and the 2016 Zika outbreak. Once COVID-19 began, like most organizations, all but the most critical non-COVID work was put on hold. “Our work practices changed to maximize telework and social distancing for laboratory work, working in shared spaces felt more like working in the BSL-3 laboratory,” said Schiffer.
Schiffer changed jobs in October, where most of his current work is not COVID-related, but instead, looking at ways to improve laboratory preparedness for emergency responses across CDC, and in state and local public health laboratories. The one exception is the new collaboration with Operation Warp Speed on a non-human primate trial to try to establish a correlate of protection for COVID vaccines.
In August 2020, Schiffer enrolled in USF Health’s DrPH program. He originally was concentrating in Clinical Laboratory Science and Practice but has since switched to Advanced Practice Leadership to better suit his change in jobs. His educational background includes a Bachelor of Arts in Molecular Biology and a Master of Science in Biology. “While my Biology background and experience is strong, I do a lot of collaborations with epidemiologists,” said Schiffer. “I have learned on the job what I needed for each project with them, but always felt that I had gaps in my knowledge of epidemiology in general.” Schiffer had been looking for several years for some type of doctoral program, but most required either on-site or full-time learning, and he did not want to leave his current job. “The USF program is the first one I found that was both highly rated and feasible to do while working full time,” said Schiffer. The DrPH program is his first experience with extensive online remote learning, but thanks to COVID, his youngest is also using Canvas for virtual high school, so they’re learning to navigate online school together.
The courses in the DrPH program are already making a difference in Schiffer’s career, as he was able to make useful contributions towards the CDC’s new framework for Public Health Preparedness and Response research, with emphasis on a systems approach and improving health equity, without having to first play catch-up on those issues. Schiffer also excitedly recalls that the gap in his research toolbox is already shrinking because, “in a recent meeting with our extramural research director she started talking about the social determinants of health, and thanks to my first semester courses I actually knew what she was talking about.”
 Jennifer Gunderman, MPH
Jennifer Gunderman, MPH
Director of the Maine Area Health Education Center (AHEC), University of New England
PORTLAND, ME – As a leader in workforce development with specific focus on rural and underserved communities, the work of the Maine AHEC Network highlights the strengths, challenges, and opportunities faced by populations vulnerable to health disparities. “COVID-19 has not changed my role, just the urgency in which things need to get accomplished,” said Gunderman.
The Maine AHEC Network has used CARES Act funds for health profession education programs to promote the use of telehealth technologies and continue its mission to provide workforce development opportunities while enhancing the prevention, preparation, and response to COVID-19. Preparation activities have included Project ECHO programming, trainings at health profession schools, and continuing education on self-care and resiliency. UNE has recently become a Project ECHO hub and AHEC staff have completed training to implement ECHO sessions. The Program Office is working with students in health profession programs to offer COVID-19 related training on PPE, screening, testing, treatment, and control measures. “None of the work of Maine AHEC could be done on our own,” said Gunderman. “We rely on networks of health care, public health, community-based organizations, private partnerships, governmental agencies, etc. Our work revolves around interprofessional and multisector collaborations. It takes a system to create sustainable change.”
The Program Office and Regional Centers is collaborating with health systems, Maine Chapters of healthcare affiliations, and others to offer continuing education opportunities to healthcare professionals related to self-care, resiliency, and mental health first aid. The Program Office is also partnering with Gateway Community Services, a community-based program serving refugees and immigrants, to assess the impact of COVID 19 on the community of immigrants and refugees and to identify ways to improve health outcomes.
In September 2020, Gunderman enrolled in USF Health’s DrPH program with a concentration in Advanced Practice Leadership. “I wanted to become the student,” said Gunderman. “I feel like I have reached a point in my personal and professional life that my skills could be enhanced and strengthened to have greater impact on public health.”
Her educational background includes a Bachelor of Science in Health Policy and Management from Providence College in Rhode Island, and a Master’s in Public Health with a certificate in Maternal and Child Health Epidemiology from Emory University in Georgia. Gunderman chose the University of South Florida for her DrPH because of the focus in leadership development and public health practice within the context of application in the real world. “I appreciate the general care the faculty and staff have for the students and creating an authentic learning environment,” said Gunderman. “While I am still in my first semester, the course work has been immediately applicable to my work. The models and concepts taught by Dr. Levine has been immediately applied to enhancing my leadership style as I guide my team of staff through these unprecedented times. What I have learned about social marketing in Dr. Pasha’s class has allowed me to use this framework when talking about addressing the infodemic related to COVID-19. I even included it in a panel in which I participated.”
The work of public health professionals is often happening behind the scenes, but COVID-19 pushed it to the forefront and turned on a spotlight for the general public to have a better understanding of what public health does and its important role in our world. “Public health is in everything,” said Gunderman. “With public health’s foundation in equity and justice and basis in science, the core principles and values should be applied to just about anything we do in this world.”

Sarah Scharf, MPH
Founding Member and Chief Administrative Officer of MD1 Program
NEW BRUNSWICK, NJ – While working full time at Rutgers University as Program Manager of Population Sciences in Administration and Planning at Rutgers Cancer Institute, Scharf helped found as a 501c3, the MD1 Program. MD1 specializes in bringing 24/7, immediate life-saving care to the scene of an incident when patients are unable to get to the hospital such as in the case of entrapment or a mass casualty incident. In regards to COVID-19, MD1 has also trained more than 120 first responders on the proper use of personal protective equipment (PPE), helped facilitate logistics for various testing and vaccination programs in New Jersey and across the United States and intubated patients while wearing powered air purifying respirators (PAPRs) in order to reduce risk of viral transmission to paramedics. “COVID has pivoted our life saving model. With fewer cars on the road, fewer citizens out and about and fewer flights in the skies, COVID has become a main focus of our life saving endeavors, especially during the peak of the pandemic in the NJ/NY area,” said Scharf.
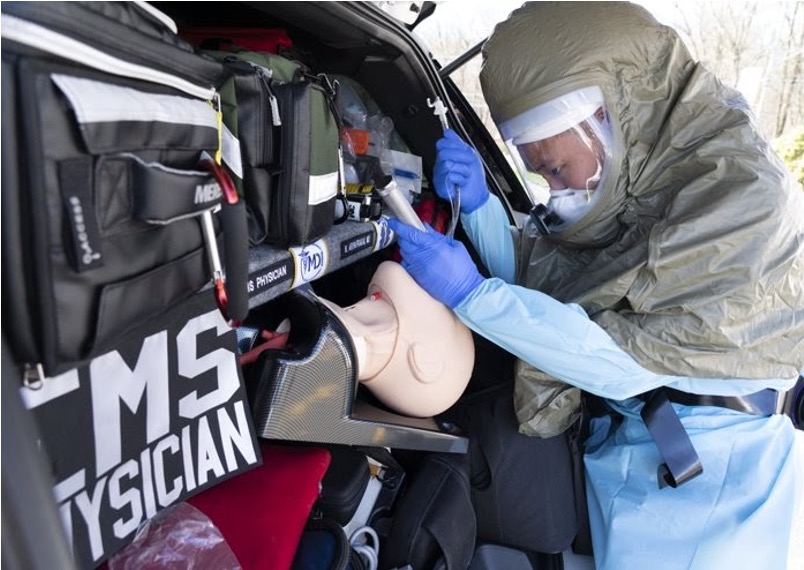
An MD1 doctor demonstrating intubation while wearing a Powered Air Purifying Respirator (PAPR). (Photo courtesy of Scharf)
In August 2020, Scharf enrolled in USF Health’s DrPH program with a concentration in Advanced Practice Leadership. Her educational background includes a Master’s in Public Health from Rutgers University. “The field of public health is rapidly expanding due to several factors and will continue even more so to need passionate, dedicated and trained individuals,” said Scharf. “I decided to pursue a DrPH to gain new perspectives, insights, and techniques to build upon my current skill set. I hope to develop advanced problem-solving skills and help strengthen my credibility as well as increase opportunities.” She chose to continue her education at USF because the program is ranked among the top 5 online DrPH programs. So far, Scharf has been enjoying the intellectually rich environment, passion and expertise of the faculty and diverse group of cohorts, and she looks forward to the day when it’s safe to meet some of her classmates in person.
“Ultimately my aim as a public health professional is to promote and protect the health of people and the communities where they live, learn, work, and play,” said Scharf. “I wholeheartedly believe this Doctorate of Public Health in Advanced Practice Leadership will help me become a better leader and make a greater impact towards the overall betterment of society. I am truly honored to have been accepted into this program and look forward to this enriching journey.”

An MD1 EMS Physician on the scene of a car accident. (Photo courtesy of Scharf)
 Alida Gertz, MD, MPH, MSc
Alida Gertz, MD, MPH, MSc
Core Faculty in the Family Medicine Residency Program, WellStar Healthcare System
ATLANTA, GA – Dr. Gertz is a Board-Certified Family Physician and helps to take care of patients in outpatient clinics and hospitals in the WellStar Healthcare System. Since COVID-19, her calendar became a bit more packed with multiple weekly team meetings about implementing new safety protocols for the family medicine outpatient clinic, reviewing current literature for clinical care of patients in the hospital with COVID-19 and discussing, approving and guiding COVID-19 research conducted within WellStar hospital and clinic. “The decisions we make have a direct impact on the care given to our patients,” Dr. Gertz said. “One of the biggest challenges is people are really scared of COVID-19, including our staff.” One decision that was presented at the outpatient clinic faculty meeting was whether COVID-19 testing should be offered at the clinic. While offering rapid testing breaks now barriers to access for patients, it also encourages potentially COVID-positive patients to come to the clinic, putting the staff, residents and students at risk. Once the clinic’s team determined that they had the proper protocols in place, such as enough personal protective equipment (PPE), they ultimately made the decision to offer COVID-19 testing.
Another challenge was the clinic normally offered home visits which was a critical way to reach the more vulnerable populations such as the working-class African Americans and Hispanic, Latinx and Vietnamese immigrants living just South of Atlanta. Like for many healthcare systems, COVID-19 pushed WellStar’s telehealth platform to be rolled out across the entire healthcare system instead of its previously limited availability. Unfortunately, telehealth often leaves out the more vulnerable populations and so the clinic staff are, “trying really hard to continue to offer them services, but in a safe way for the staff,” Dr. Gertz said.
Dr. Gertz’s educational background includes a Medical Degree and Master of Public Health from Case Western Reserve University and a Master of Science in Epidemiology and a Professional Diploma in Tropical Medicine and Hygiene from the London School of Hygiene and Tropical Medicine. She completed two years of Internal Medicine residency at Johns Hopkins University, and two years of Family Medicine residency at the University of Pennsylvania and a Global Health Fellowship at the University of Washington and another through Harvard TH Chan School of Public Health. Dr. Gertz decided to pursue a DrPH with a concentration in Advanced Practice Leadership, because she was interested in transitioning to a career in public health and while she already has an MPH, she wanted a more solid, formal training in public health as well as additional experience and training in statistics and particularly using SAS
While completing her first semester of the DrPH program, Dr. Gertz is developing an anti-racism curriculum for her resident students at WellStar. “I received input from my professors on the best way to develop the program so that it is grounded in research and the curriculum can be evaluated in a meaningful way,” Dr. Gertz said. “It wouldn’t have been as well designed without the supervision and guidance from my professors because it wouldn’t have been done in such a systematic and structured way.” The assignments in the program are often directly or indirectly influenced by the pandemic and Dr. Gertz notes that she feels a unique sense of urgency to complete her work because the research can influence the current state of affairs. For example, in her Social Marketing course, she is on a team that is focusing on decreasing COVID-19 vaccine hesitancy among African Americans.
Already following through with her desire to transition to a career in public health, Dr. Gertz recently accepted a position with the CDC in the Division of Global Migration and Quarantine. According to the CDC, their mission is to, “reduce morbidity and mortality among immigrants, refugees, travelers, expatriates, and other globally mobile populations, and to prevent the introduction, transmission, and spread of communicable diseases through regulation, science, research, preparedness, and response.” COVID-19 created the need for a team member specifically dedicated to COVID-19 protocols and that will soon be Dr. Gertz’s role. The job is based out of the Hartsfield-Jackson Atlanta International Airport and focuses on traveler health for various major airports in the U.S. as well as for a number of seaports.
While each student shares a desire to gain more knowledge and expertise in the public health field, each student has their own specific interests and different needs. Even just one semester into the program, Dr. Gertz appreciates the individualized attention she has received from the supportive and responsive faculty. “The faculty are kind and caring and very knowledgeable about their areas of expertise. They each bring their own perspective and a lot of experience,” Dr. Gertz said.
